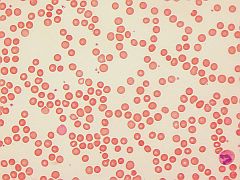
(BMJ)—A 41-yo woman presented w/ a 3-day hx of fever, cough, yellow eyes, and left upper quadrant pain. Three similar episodes in the past 5y each resolved w/ abx. Exam: pallor, scleral icterus. Spleen: tender, enlarged. Labs: Hgb decreased; WBC elevated; platelets WNL; absolute reticulocyte count elevated; indirect bilirubin elevated; liver enzymes WNL; direct antiglobulin negative. What is the dx?
|
Cholecystitis
|
|
Malaria
|
|
Autoimmune hemolytic anemia
|
|
Hereditary spherocytosis
|
|
Gilbert syndrome
|
