-
For DKA,1 replace fluids; manage K+; start insulin drip; monitor BG, labs - Fluids: normal saline 1L/h x1-3h,2 then NS or ½ NS (base2 on corrected Na+ 3) at 250-500 cc/h. Once BG reaches 200 mg/dL: Switch to ½ NS w/ 5%-10% dextrose @150-250 cc/h
- HCO3: Consider giving if pH <7, HCO3 <10 mEq/L, K+ >6.5 mEq/L w/ EKG changes, or K+ >7 mEq/L
- K+ goal: 4-5 mEq/L. If K+ <3.3 mEq/L give 20-40 mEq/h; if K+ 3.3-5.3 mEq/L give 20-30 mEq K+ per L IV fluid; if K+ >5.3, then ✓ K+ q2h
- Labs: ✓basic lytes, serum osmolality and venous/arterial pH q2-4h (✓lytes q2h if K+ being replaced)
Start insulin drip, aim for BG 140-180 mg/dL;4 monitor BG - Don’t give insulin until K+ ≥3.3 mEq/L
- Regular insulin: 0.1 unit/kg bolus, then 0.1 unit/kg/h drip (alt: skip bolus, 0.14 unit/kg/h infusion)
- ✓BG q1h until BG stable in target range,4 then q2h
- If BG drop/h is <50 mg/dL: bolus 0.1 unit/kg q1h until BG ↓ by ≥50 mg/dL/h
- If BG drop/h is 50-100 mg/dL: Continue current infusion
- If BG drop/h >100 mg/dL: ↓ insulin drip rate by 50%
- Once BG ≤200 mg/dL: ↓ insulin infusion rate by 50% and add dextrose to IV fluids
Transition to SC insulin, allowing 2h overlap5 w/ insulin drip - Readiness: BG <200 mg/dL, HCO3 ≥15 mEq/L, anion gap <12 mEq/L, no IV vasoconstricting meds, not intubated, able to tolerate nutrition intake
- Calculate daily insulin requirement6 based on drip; overlap5 SC insulin with drip; make daily adjustments
- Avoid/tx hypoglycemia7 (BG <70 mg/dL): Eval risk factors,8 prescribing errors, nutritional mismatch9
Footnotes 1 DKA lab dx: serum glucose >250 mg/dL; pH <7.3 w/ HCO3 <18 mEq/L, anion gap; ↑serum ketones. Clinical: dehydration, vomiting, abd pain, etc.
2 Fluid replacement in 3 steps:
• Give isotonic saline @15-20 mL/kg lean body wt/h x1-3h
• Change fluids based on electrolyte level and clinical hydration: If corrected sodium <135 mEq/L, continue normal saline at 250-500 mL/h; if corrected sodium NL/elevated, use half-normal saline at 250-500 mL/h
• When plasma glucose reaches 200 mg/dL, change fluids to half-normal saline w/ 5%-10% dextrose at 150-250 mL/h and adjust insulin
3 Corrected Na+ = measured sodium + [(glucose mg/dL – 100) x1.6/100]
4 AACE-ADA guidelines recommend maintaining BG 140-180 mg/dL in critically ill pts; ACP recommends 140-200; SCCM recommends 100-150 w/ emphasis on avoiding hypoglycemia in critically ill pts; BG ≥150 should trigger intervention (eg, insulin drip) to keep BG <150, and absolutely below 180. Lower targets (eg, 110-140) might be appropriate for certain pts, based on limited evidence.
5 Overlap SC insulin with insulin drip. Several methods to overlap insulin infusion w/ basal insulin exist:
• Give 1st dose basal SC insulin 2-3h before infusion stopped, or
• Stop infusion, give 10% basal dose as rapid-acting along w/ basal insulin dose, or
• Give a dose of short- or rapid-acting insulin 1-2h before infusion stopped
6 Calculate SC dose from infusion: Multiply average hourly infusion rate over prior 6-8h x24, then decrease to 60%-80% of that dose. Use this value for total daily dose if pt on nutritional support (TPN or tube feeds), or as basal amount w/ nutritional-layered insulin prn as oral intake increases. Adjust doses daily.
7 ADA defines hypoglycemia <70 mg/dL, severe hypoglycemia <40 mg/dL. Tx w/ 50 mL of D50 (equivalent to 25 g carbohydrate, which ↑ BG by 125 mg/dL).
8 Hypoglycemia risk factors:
• Advanced age
• Malnutrition/cachexia/low BMI
• ESLD
• ESRD
• Sepsis
• CHF
• Multiorgan failure
• Advanced malignancy
9 If nutrition abruptly stops (eg, tube feed/TPN interrupted for transport, etc): Reduce insulin infusion rate by 50%. Unexpected interruption of nutrition intake is common:
• Discontinuation of enteral/parenteral feeds
• Taking in less than expected nutrition after nutritional insulin already delivered
• Unexpected transport from unit
-
For critically ill1 non-DKA hyperglycemia, use insulin drip; monitor BG. ✓A1c2 - ✓BG on hospital admission and when starting steroids3/TPN; if BG >140 mg/dL, keep testing for ≥24-48h
- Stop any oral/injectable noninsulin antihyperglycemics
- Start insulin drip if BG ≥180; aim for BG 140-1804 in critically ill1 pts. Divide initial BG by 100, round up/down to nearest 0.5: This value is both the bolus amount (units) and the initial infusion rate (units/h)
- ✓BG q1h while on IV insulin, until 3 consecutive values in target range, then q2h. Once stable x12-24h, ✓q4h. Resume q1h checks if: any BG out of range; insulin infusion rate change; clinical condition change; starting/stopping steroids,3 pressors, TPN/tube feed, or dialysis/CVVH/CAVH. If vasoconstricted or hypotensive, prefer venous/arterial BG testing over fingerstick
- Avoid/tx hypoglycemia5 (BG <70 mg/dL): Eval risk factors,6 prescribing errors; address nutritional mismatch7
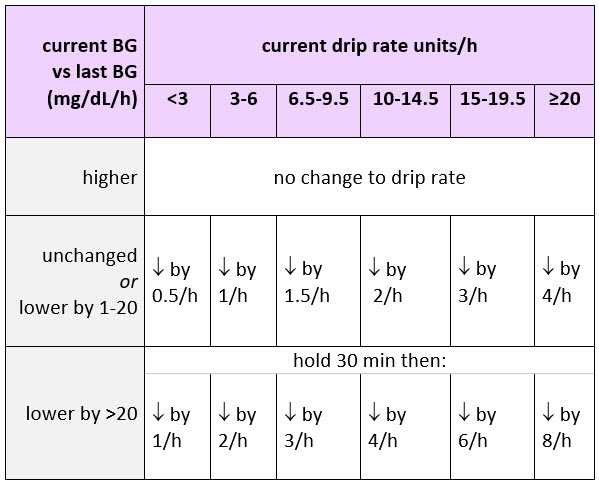
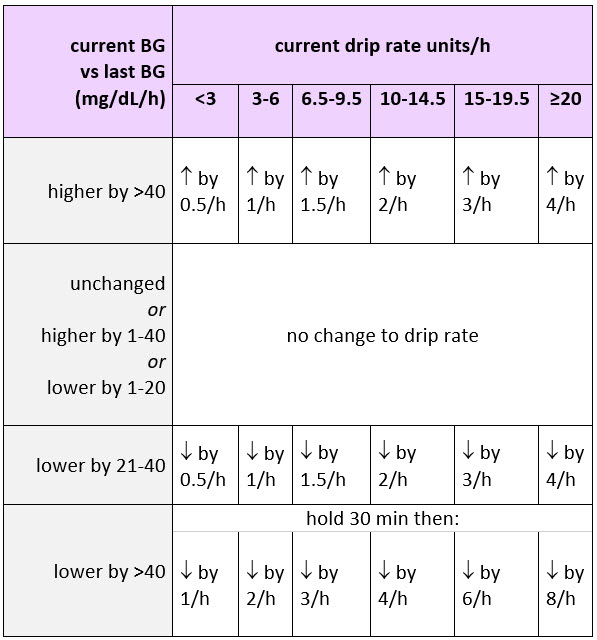
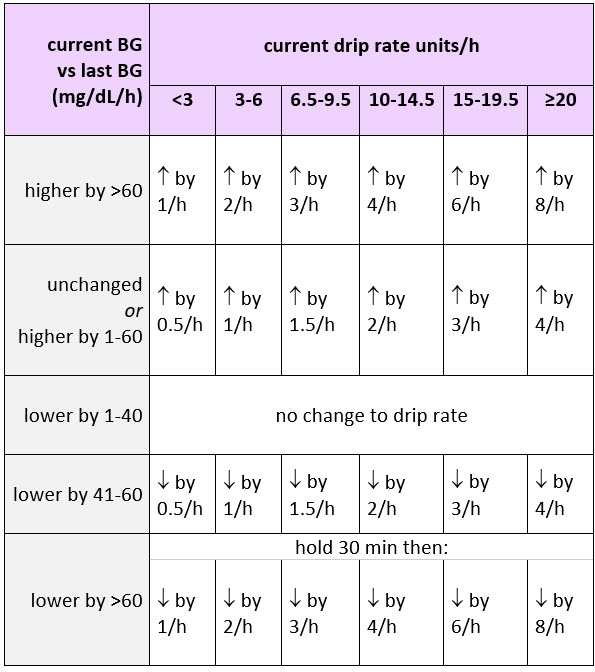
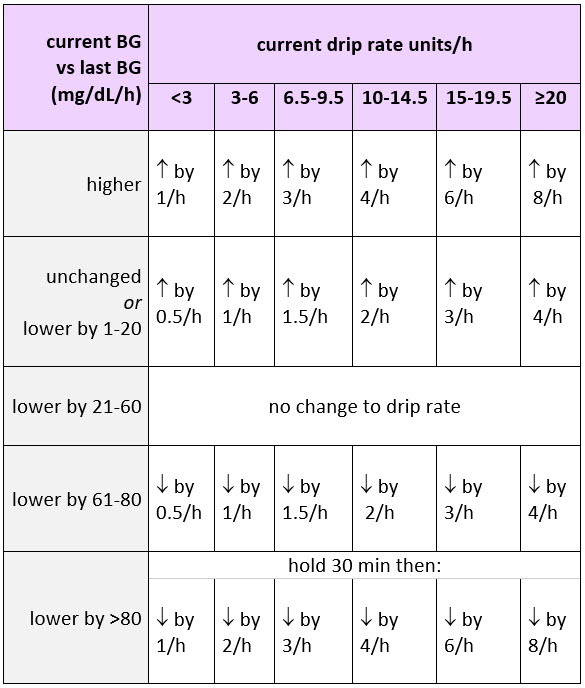
- Adjust insulin drip based on BG ✓. Once pt stable, transition to basal/bolus insulin,8 allowing 2h overlap9 w/ insulin drip, prior to d/c from ICU
If BG is ≤99: Adjust insulin drip based on current BG (mg/dL), comparing average hourly rate of change10 since last BG as follows: - If <50: d/c insulin drip, give 1 amp (25g) D50 IV, recheck BG q15min until ≥90; then recheck q1h; once ≥140 wait 30 min, then restart insulin drip @50% of most recent rate
- If 50-74: Give ½ amp (12.5 g) D50 IV; recheck BG q15min until ≥90; then recheck q1h; once ≥140 wait 30min, then restart insulin drip @50% of most recent rate
- If 75-99: Recheck BG q15min until ≥90; then recheck q1h; once ≥140 wait 30min, then restart insulin drip @75% of most recent rate
If BG is 100 to 119 mg/dL/h: Average BG change per hr.10 If BG ↓ >20/h, d/c insulin infusion, ✓BG in 15min to ensure ≥90; recheck q1h; once BG ≥140 wait 30min, then restart insulin drip @75% of most recent rate as follows: If BG is 120 to 159 mg/dL/h: Average BG change per hr as follows: If BG is 160 to 199 mg/dL/h: Average BG change per hr as follows: If BG is ≥200 mg/dL/h: Average BG change per hr as follows: Footnotes 1 Pts on invasive mechanical ventilation, on pressors, or w/ multisystem organ failure. Pts w/ DKA or hyperosmolar hyperglycemic state may require higher initial insulin dosage, IV dextrose, and adjunctive tx for fluid/electrolyte/acid-base status. Pts w/ initial BG >500 may also require higher initial insulin dosing and additional tx. Not appropriate insulin drip candidate: pts who are eating, transferring out of ICU in <24h, expected to rapidly normalize glycemic status, or pre-terminal illness/comfort measures only.
2 OK to use A1c value ~60 days prior to admission. NL A1c distinguishes stress hyperglycemia from T1/T2DM.
3 Steroids. Consider steroid infusions rather than bolus. Hyperglycemia peaks 8-12h after steroid dose.
4 AACE-ADA guidelines recommend maintaining BG 140-180 mg/dL in critically ill pts; ACP recommends 140-200; SCCM recommends 100-150 w/ emphasis on avoiding hypoglycemia in critically ill pts; BG ≥150 should trigger intervention (eg, insulin drip) to keep BG <150, and absolutely below 180. Lower targets (eg, 110-140) might be appropriate for certain pts, based on limited evidence.
5 ADA defines hypoglycemia <70 mg/dL, severe hypoglycemia <40 mg/dL. Tx w/ 50 mL of D50 (equivalent to 25 g carbohydrate, which ↑ BG by 125 mg/dL).
6 Hypoglycemia risk factors:
• Advanced age
• Malnutrition/cachexia/low BMI
• ESLD
• ESRD
• Sepsis
• CHF
• Multiorgan failure
• Advanced malignancy
7 Nutrition adjustments on insulin drip:
• If nutrition abruptly stops (eg, tube feed/TPN interrupted for transport, etc.), reduce insulin infusion rate by 50%
• Consider starting D10 @ tube feed/TPN infusion rate (caution in pts w/ cerebral edema or hyponatremia. Alternative: contact pharmacy to decrease insulin drip rate according to Insulin Sensitivity Coefficient; or stop insulin drip and start SC insulin w/ correction scale and q2-4h monitoring (eg, lispro q4h or regular insulin q6h)
• ✓BG q1h until in target range x3 consecutive readings
• If BG <70 mg/dL (or 70-79 mg/dL while symptomatic): Follow hospital hypoglycemia protocol and ✓BG w/in 15-30 min
• If on parenteral nutrition: give insulin parenterally w/ nutrition
• In the rare pt who is eating: consider SC insulin aspart pc to cover meals (1 unit/10-15g carbs) and don’t increase insulin infusion rate during 1st 3h pc
8 Transition to SC insulin all pts w/ T1DM, insulin-requiring T2DM, or any hyperglycemic requiring >1-2 unit/hr insulin:
• Readiness: BG <200 mg/dL, HCO3 ≥15 mEq/L, anion gap <12 mEq/L, no IV vasoconstricting meds, not intubated, able to tolerate nutrition intake
• Calculate subcutaneous dose from infusion: average infusion rate over prior 6-8h x24h, then decrease to 60%-80%. Use this value for total if pt receiving nutritional support (TPN or tube feeds) or as basal amount w/ nutritional layered insulin prn as oral intake increases.
• Make daily adjustments
9 Overlap SC insulin with insulin drip. Several methods to overlap insulin infusion w/ basal insulin exist:
• Give 1st dose basal SC insulin 2-3h before infusion stopped, or
• Stop infusion, give 10% basal dose as rapid-acting along w/ basal insulin dose, or
• Give a dose of short- or rapid-acting insulin 1-2h before infusion stopped
10 Compare current BG to the last BG checked, divided by time between the 2 checks, to get the average BG change per hr. -
Eating/Bolus tube feeding Basal + nutritional + correction insulin; aim for BG 100-180 for most pts;1 adjust for nutrition; stop noninsulin antihyperglycemics. ✓A1c2 - If admit BG >140 mg/dL, or if starting steroids3/TPN: Continue testing ≥24h-48h
- D/C noninsulin antihyperglycemic agents, though certain T2DM pts4 may continue oral agents + only correctional insulin
- Treat hyperglycemia (T1DM, T2DM, etc) w/ SC insulin. Distribute estimated total daily dose:5 50% long-acting basal (once daily) + 50% rapid-acting6 nutritional (divide equally pre-meal/bolus feed)
- Basal: Insulin glargine or detemir preferred for once-daily basal in nonpregnant 7 pts
- Nutritional: Rapid-acting6 (eg, lispro) preferred; give w/in 15min of 1st bite of meal or bolus start. If nausea/poor appetite, adjust insulin timing by up to 30min and account for portion of meal8
- Correctional: Specify correction9 rapid-acting SC insulin (eg, lispro) based on estimated insulin sensitivity
- ✓BG 4x/day: qac, qhs. Repeat ✓ if meal not delivered w/in 30min of premeal BG ✓
- Adjust daily: Add up previous day’s correction insulin, redistribute equally to basal and nutritional doses. If any BG >180 w/ no hypoglycemia threat, increase total daily dose by 10%-20%; if BG consistently >180-200, increase total daily dose by 30%. If BG <100 mg/dL, consider reducing insulin by 20%-30%; if any hypoglycemia (eg, <70), decrease by 50% and consider D51/2NS @75 cc/h
- Consider pumps/infusions. Consider insulin infusion if uncontrolled hyperglycemia on steroids3 or TPN, hyperglycemic crisis, or L&D. If T1DM managed on insulin pump as outpt, consider continuing as inpt if criteria met.10 If pregnant: OK to continue insulin pump
- Avoid/tx hypoglycemia11 (BG <70 mg/dL): Eval risk factors,1 prescribing errors, nutritional mismatch8
Adjust for changing nutrition intake8 - Diet: consistent controlled carbs. Snacks not automatically required; offer low/no carb snacks, additional nutritional insulin coverage may be needed for carb-containing snacks
- If bolus tube feed: Give insulin immediately before or immediately after nutrition delivery8
- Hold nutritional insulin when nutrition interrupted8
- If malnutrition, obesity: Consider nutritionist consultation
Footnotes 1 Higher targets OK if hypoglycemia risk factors: advanced age, terminally ill/advanced malignancy, malnutrition/cachexia/low BMI, severe comorbidities (ESKD, ESLD, CHF, multiorgan failure, sepsis), or where monitoring/nurse supervision not available. Lower targets occasionally appropriate if clinically stable w/ successful hx of tight control.
2 OK to use A1c value ~60 days prior to admission. NL A1c distinguishes stress hyperglycemia from T1/T2DM.
3 Steroids. Consider steroid infusions rather than bolus. Hyperglycemia peaks 8-12h after steroid dose. NPH insulin (alone or layered on other insulin) works well; or keep basal insulin consistent while escalating rapid-acting insulin at lunch and dinner to address postprandial effects of steroids. Consider endocrine consult.
4 Initial tx w/correctional insulin only may be appropriate in T2DM if:
• Well-controlled (A1c <7% or normal BG values) w/ diet only or low-dose oral agent, and have
• Mild hyperglycemia plus one/more of these:
-NPO w/o nutritional replacement
-on new/tapering steroids
-have hypoglycemic risk factors (eg, ESLD/ESLD dz, elderly, unknown drug overdose, etc)
5 Base on body habitus, considering A1c, hypoglycemia risks, etc
• NL habitus standard: 0.4 units/kg/day
• Very lean, on HD, or very insulin sensitive (hypoglycemia risk factors): 0.3 units/kg/day
• Overweight/obese. If overweight: 0.5 units/kg/day; if obese or known insulin-resistance: 0.6 units/kg/day (or more)
Review prescribed home meds, med adherence, A1c, hx hypoglycemia
• If adherent on fixed-split or basal-only insulin at home: Change to basal/bolus, w/ 50% basal and 50% meal-time bolus (+ correctional scale)
• If nonadherent on insulin at home: Use wt-based estimate or 1/2 home dose to start, w/ correctional scale layered on top
If transitioning from IV insulin infusion, take average hourly rate over last 6h, multiply by 20
• If previously eating/tube feeds/TPN/on D5 IV: Use this value as estimated total daily dose
• If insignificant nutrition over last 6h, double this value for estimated total daily dose
6 Insulin “stacking” can occur w/ regular insulin; if regular insulin used, reduce or eliminate lunchtime dose.
7 NPH considered standard of care for diabetes in pregnancy.
8 If unexpected interruption of nutritional intake (eg, d/c tube feed, poor intake, transportation from area): Adjust nutritional insulin.
If poor appetite: Give nutritional dose up to 30min after 1st bite/tube feed bolus start:
• Give no nutritional insulin if <50% of meal
• Give half dose if pt ate 50%
• Give full dose if pt ate >50% of meal
If on insulin drip:
• If nutrition stopped/interrupted after glargine insulin given in last 24h (or NPH in last 12h): start D10 IV fluid at the tube feed/TPN infusion rate (caution in pts w/ cerebral edema or hyponatremia). Then d/c in D10 IV fluid 24h after last glargine dose (12h after last NPH dose), or when enteral nutrition restarted. Alternative: Contact pharmacy to decrease insulin drip rate according to Insulin Sensitivity Coefficient; or stop insulin drip and start SC insulin w/ correction insulin scale and q2-4h monitoring
• ✓BG q1h until in target range x3 consecutive readings
• If BG <70 mg/dL (or 70-79 mg/dL while symptomatic): Follow hospital hypoglycemia protocol and ✓BG w/in 15-30min
If on SC insulin:
• If on glargine: continue glargine, consider reducing dose by 20% if tight control or at high risk for hypoglycemia
• If on regular scheduled nutritional insulin (regular or lispro): If nutritional dose was given in past 1-6h, increase frequency of BG ✓ to q1-2h until insulin action complete; hold future nutritional insulin until nutrition resumes, but continue correction insulin
• If BG <70 mg/dL (or 70-79 mg/dL while symptomatic): Follow hospital hypoglycemia protocol and ✓BG w/in 15-30min
• Consider starting D10 IV fluid at tube feed/TPN infusion rate
• ✓BG q4-6h and prn
9 Use same insulin type for correction as for nutritional (eg, rapid-acting); in eating/tube feed pts, reduce nocturnal correction doses.
10 If pump tx interrupted for >1h, insulin drip or SC basal/bolus must be used.
Contraindications of pt self-management of insulin pump:
• Altered level of consciousness/ cognition impairment
• On meds that alter state of consciousness
• Impaired judgment/ suicide risk
• Uncontrolled BG trends/ acute situations (eg, DKA) for which pt/caregiver can’t make appropriate self-adjustments to basal/bolus doses
• Insulin pump not working properly or pump supplies not available
• Pt/Caregiver refusal/inability to participate in pump tx, or refusal to comply w/ necessary requirements in institution’s pump policy
11 ADA defines hypoglycemia <70 mg/dL, severe hypoglycemia <40 mg/dL. Tx w/ 50 mL of D50 (equivalent to 25 g carbohydrate, which ↑ BG by 125 mg/dL). Hypoglycemic risk factors: advanced age, malnutrition/cachexia/low BMI, ESLD, ESRD, sepsis, CHF, multiorgan failure, advanced malignancy.
Continuous tube feeding/Parenteral nutrition Basal + nutritional + correction insulin, aim for BG 100-180 for most pts;1 adjust for nutrition; stop noninsulin antihyperglycemics. ✓A1c2 - ✓BG on hospital admission and if starting steroids3/TPN; if BG >140 mg/dL, ongoing testing for ≥24h-48h
- Stop any oral/injectable noninsulin hyperglycemics
- SC insulin: Calculate total daily dose4
- If continuous tube feeds: Administer 40%-50% as basal insulin (once-daily, glargine preferred), 50%-60% as nutritional insulin (regular insulin, preferred, q6h)
- If TPN: Start separate insulin drip to find dose, then add regular insulin to subsequent TPN bags
- Specify correctional insulin, using same insulin type as nutritional insulin; base on insulin sensitivity
- Consider insulin drip for optimal control; consider insulin pump in select cases
- Monitor BG q6h. Avoid/tx hyperglycemia5 (BG <70 mg/dL)
- If tube feeds or parenteral nutrition held/interrupted,6 also hold nutritional doses
Footnotes 1 Higher targets OK if hypoglycemia risk factors: advanced age, terminally ill/advanced malignancy, malnutrition/cachexia/low BMI, severe comorbidities (ESKD, ESLD, CHF, multiorgan failure, sepsis), or where monitoring/nurse supervision not available. Lower targets occasionally appropriate if clinically stable w/ successful hx of tight control.
2 OK to use A1c value ~60 days prior to admission. NL A1c distinguishes stress hyperglycemia from T1/T2DM.
3 Steroids. Consider steroid infusions rather than bolus. Hyperglycemia peaks 8-12h after steroid dose. NPH insulin (alone or layered on other insulin) works well; or keep basal insulin consistent while escalating rapid-acting insulin at lunch and dinner to address postprandial effects of steroids. Consider endocrine consult.
4 Base on body habitus, considering A1c, hypoglycemia risks, etc
• NL habitus standard: 0.4 units/kg/day
• Very lean, on HD, or very insulin sensitive (hypoglycemia risk factors): 0.3 units/kg/day
• Overweight/obese. If overweight: 0.5 units/kg/day; if obese or known insulin-resistance: 0.6 units/kg/day (or more)
Review prescribed home meds, med adherence, A1c, hx hypoglycemia.
• If adherent on fixed-split or basal-only insulin at home: Change to basal/bolus
• If nonadherent on insulin at home: Use wt-based estimate or 1/2 home dose to start, w/ correctional scale layered on top
If transitioning from IV insulin infusion, take average hourly rate over last 6h, multiply by 20
• If previously eating/tube feeds/TPN/on D5 IV: Use this value as estimated total daily dose
• If insignificant nutrition over last 6h, double this value for estimated total daily dose
5 ADA defines hypoglycemia <70 mg/dL, severe hypoglycemia <40 mg/dL. Tx w/ 50 mL of D50 (equivalent to 25 g carbohydrate, which ↑ BG by 125 mg/dL). Hypoglycemic risk factors: advanced age, malnutrition/cachexia/low body mass, ESLD, ESRD, sepsis, CHF, multiorgan failure, advanced malignancy.
6 Hold nutritional insulin when nutrition interrupted (eg, d/c tube feed/parenteral nutrition, transportation from area).
If on insulin drip:
• If nutrition stopped/interrupted after glargine insulin given in last 24h (or NPH in last 12h): start D10 IV fluid at the tube feed/TPN infusion rate (caution in pts w/ cerebral edema or hyponatremia). Then d/c in D10 IV fluid 24h after last glargine dose (12h after last NPH dose), or when enteral nutrition restarted. Alternative: Contact pharmacy to decrease insulin drip rate according to Insulin Sensitivity Coefficient; or stop insulin drip and start SC insulin w/ correction insulin scale and q2-4h monitoring
• ✓BG q1h until in target range x3 consecutive readings
• If BG <70 mg/dL (or 70-79 mg/dL while symptomatic): Follow hospital hypoglycemia protocol and ✓BG w/in 15-30min
If on SC insulin:
• If on glargine: Continue glargine, consider reducing dose by 20% if tight control or at high risk for hypoglycemia
• If on regular scheduled nutritional insulin (regular or lispro): If nutritional dose was given in past 1-6h, increase frequency of BG ✓ to q1-2h until insulin action complete; hold future nutritional insulin until nutrition resumes, but continue correction insulin
• If BG <70 mg/dL (or 70-79 mg/dL while symptomatic): Follow hospital hypoglycemia protocol and ✓BG w/in 15-30min
• Consider starting D10 at tube feed/TPN infusion rate
• Resume q4-6h and prn BG ✓
If on zero carbs: Use basal + correction insulin, w/o nutritional insulin; aim for BG 100-180 for most pts;1 stop noninsulin antihyperglycemics. ✓A1c2 - ✓BG on hospital admission and if starting steroids or TPN; if BG >140 mg/dL, ongoing testing for ≥24h-48h
- Stop any oral/injectable noninsulin antihyperglycemics
- SC insulin: Calculate total daily dose;3 administer 50% as basal (glargine preferred) once daily. No nutritional insulin needed
- Specify correction scale q6h w/ regular insulin if NPO >24h;4 base on insulin sensitivity
- If T1DM on prolonged fast: Manage w/ IV insulin infusion
- Consider D5-containing drip at 75-150 mL/h, esp if hypoglycemia risk and/or prolonged NPO
- ✓BG either qac/qhs or 6h if using regular insulin (q4h if using rapid-acting). Avoid/tx hypoglycemia1,5
Footnotes 1 Higher targets OK if hypoglycemia risk factors: advanced age, terminally ill/advanced malignancy, malnutrition/cachexia/low BMI, severe comorbidities (ESKD, ESLD, CHF, multiorgan failure, sepsis), or where monitoring/nurse supervision not available. Lower targets occasionally appropriate if clinically stable w/ successful hx of tight control.
2 OK to use A1c value ~60 days prior to admission. NL A1c distinguishes stress hyperglycemia from T1/T2DM.
3 Basal insulin required for all T1DM and most T2DM, even when NPO, due to hepatic gluconeogenesis. Base on body habitus, considering A1c, hypoglycemia risks, etc.
• NL habitus standard: 0.4 units/kg/day
• Very lean, on HD, or very insulin sensitive (hypoglycemia risk factors): 0.3 units/kg/day
• Overweight/obese. If overweight: 0.5 units/kg/day; if obese or known insulin-resistance: 0.6 units/kg/day (or more)
Review prescribed home meds, med adherence, A1c, hx hypoglycemia.
• If adherent on fixed-split or basal-only insulin at home: change to 50% of total daily dose, as once-daily SC basal insulin
• If nonadherent on insulin at home: use wt-based estimate or 1/2 home dose to start, w/ correctional scale layered on top
If transitioning from IV insulin infusion, take average hourly rate over last 6h, multiply by 20.
• If previously eating/tube feeds/TPN/on D5 IV: Use this value as estimated total daily dose
• If insignificant nutrition over last 6h, double this value for estimated total daily dose
4 If NPO <24h, lispro OK.
5 ADA defines hypoglycemia <70 mg/dL, severe hypoglycemia <40 mg/dL. Tx w/ 50 mL of D50 (equivalent to 25 g carbohydrate, which ↑ BG by 125 mg/dL). Hypoglycemic risk factors: advanced age, malnutrition/cachexia/low BMI, ESLD, ESRD, sepsis, CHF, multiorgan failure, advanced malignancy.
-
Prepare home program, educate, provide supplies, arrange f/u
- If stress hyperglycemia only (A1c <5.7): ✓outpt fasting BG and GTT
- If newly detected hyperglycemia w/ A1c ≥5.7%, base home regimen1 on A1c
- If known DM w/ acceptable preadmission glycemic control w/o new contraindications: resume preadmission regimen
- If known DM not @ goal2 pre-admission, escalate/descalate home regimen2
- If prescribing oral antihyperglycemics: Withhold until day of d/c (or 1st day home)
- If prescribing insulin: Determine dose for basal3 or basal + nutritional strategy;4 start new regimen at least 1day5 prior to d/c, to assess efficacy
- Ensure adequate supplies (eg, insulin pen/syringes; BG meter, strips; lancing device, lancets; glucagon kit (if on insulin); urine ketone strip (T1DM); medical alert info
- DM teaching before discharge, including written materials specifying BG checks (at least 2x/day initially), adjustments/actions based on BG, community resources
- Schedule f/u (at least by phone): w/in 1wk if insulin started, otherwise w/in 1mo
- Consider Endocrine/Diabetes consult for mgmt/ed, esp if BG difficult to control
Footnotes 1 New hyperglycemia. Manage based on A1c level:
• 5.7-6.4% Pre-diabetes. Lifestyle change; if multiple risk factors, consider metformin or other drugs
• 6.4-7.4% Newly dx DM. Lifestyle + metformin
• 7.5-9.0% Newly dx DM, uncontrolled. Lifestyle + mono- or dual-therapy
• 9-10% Newly dx DM, uncontrolled. Lifestyle + double- or triple-therapy
• 10% Newly dx DM, uncontrolled. Lifestyle + metformin + basal/nutritional insulin preferred, esp if symptomatic; after glucose toxicity resolve, may transition to PO drugs
2 Known DM. Manage based on A1c level:
• <5.7: Assess any pre-admit hypoglycemia; de-escalate home regimen if needed
• 5.7-7.4% Controlled DM
• 7.5-9.0% Uncontrolled DM. Lifestyle + dual-therapy
• 9-10% Uncontrolled DM. Lifestyle + triple-therapy
• 10% Uncontrolled DM. Lifestyle + metformin + basal/nutritional insulin preferred, esp if symptomatic; after glucose toxicity resolves, may transition to PO drugs
3 Pts started on insulin @ d/c should have f/u, at least by phone, w/in 1wk.
If basal (w/o nutritional) insulin: 3 options for determining dose (for use w/ or w/o other med types)
• D/C mealtime bolus insulin, but continue the same dose of basal insulin, or
• Start 10 units basal insulin qhs, or
• Start 0.1-0.3 units/kg basal insulin qhs
Once pt discharged: if am fasting BG >100 mg/dL, then long-acting basal insulin can be safely increased by 2 units q3days, in pts w/ Cr <2 mg/dL. Pts started on insulin @ d/c should have follow-up, at least by phone, w/in 1wk.
4 Pts started on insulin @ d/c should have f/u, at least by phone, w/in 1wk. If pt will be on nutritional insulin, D/C insulin secretagogues.
If basal + nutritional insulin, 3 options for determining dose (w/ or w/o other meds):
• Continue hospital regimen of insulin qid: once-daily basal + 3 nutritional doses; if switching from long-acting insulin to intermediate and short-acting, dose adjustments will be required, or
• Continue hospital basal insulin + 1 nutritional dose w/ largest meal of day only, or
• Prescribe bid split mixed insulin (eg, 70/30 or 75/25)
5 If not feasible to start 1day prior d/c, consider less stringent glycemic control w/ lower initial basal insulin dose during transition, w/ rapid-acting insulin for correction doses, and increased BG monitoring.
-
Perioperative: pre-/intra-/post-op
✓A1c, screen nearly all pts for hyperglycemia; adjust meds at home1,2 before elective surgery/procedure - ✓A1c w/in 60-90days of surgery, if known DM. Consider A1c ✓ if BMI >30 or age >40 yo
- If elevated A1c and surgery elective: PCP/endocrinologist manages new hyperglycemia1 or known DM2 for wks/months pre-op if possible, until A1c closer to goal (eg, 8.5% or other goal)
- Schedule procedure in early AM for least impact on insulin dosing
Plan day before/day of surgery: Specify med adjustments if known DM, specify PO intake: T1DM pts (require insulin even when NPO) - Basal glargine or detemir. Give usual basal insulin day before and day of surgery; though for safety margin, consider ↓ dose by 20% on surgery day, esp if pt under tight control
- NPH. On morning of procedure give 1/2-2/3 usual dose
- Short-acting insulins:3 Don’t give on day of surgery, unless BG >200 mg/dL3
- Day of surgery strategy: Start insulin drip and maintain at 1-2 units/h w/ D5W at 75-100 cc/h, to maintain BG 100-180
T2DM pts: Guidelines suggest not taking oral antihyperglycemics and noninsulin injectables on day of surgery, though research not strong - Metformin: For sustained release forms, hold starting evening before procedure; for regular form, hold starting day of procedure; resume metformin 48h post-op if NL renal fxn
- Oral agents that can cause hypoglycemia (sulfonylurea, DPP4 inhibitor/other insulin secretagogue): Hold on day of surgery, resume w/ NL diet
- Alpha-glucosidase inhibitor or GLP-1 agonist (exenatide): Hold on day of procedure until eating again
- TZDs: If pills allowed, OK to continue
- Glargine or detemir: Give usual basal insulin day before and day of surgery; though for safety margin, consider ↓ dose by 20%, on surgery day, esp if pt under tight control
- NPH: On morning of procedure, give 1/2 to 2/3 of usual dose
- Short-acting insulins. Don’t give on day of surgery, unless BG>200 mg/dL3
- Day of surgery strategy: If on insulin, use insulin drip maintained at 1-2 units/h4 w/ D5W at 50-75 cc/h, to maintain BG 100-150 mg/dL
Footnotes 1 New hyperglycemia. Manage based on A1c level:
• 5.7%-6.4% Pre-diabetes. Lifestyle change; if multiple risk factors, consider metformin or other drugs
• 6.4%-7.4% Newly dx DM. Lifestyle + metformin
• 7.5%-9.0% Newly dx DM, uncontrolled. Lifestyle + mono- or dual-therapy
• 9%-10% Newly dx DM, uncontrolled. Lifestyle + double- or triple-therapy
• 10% Newly dx DM, uncontrolled. Lifestyle + metformin + basal/nutritional insulin preferred, esp if symptomatic; after glucose toxicity resolve, may transition to PO drugs
2 Known DM. Manage based on A1c level:
• <5.7%: Assess any pre-admit hypoglycemia; de-escalate home regimen if needed
• 5.7%-7.4% Controlled DM
• 7.5%-9.0% Uncontrolled DM. Lifestyle + dual-therapy
• 9%-10% Uncontrolled DM. Lifestyle + triple-therapy
• 10% Uncontrolled DM. Lifestyle + metformin + basal/nutritional insulin preferred, esp if symptomatic; after glucose toxicity resolves, may transition to PO drugs
3 Short-acting insulin (eg, lispro, aspart, glulisine): If BG >200, then use small doses (eg, 1-4 units) aiming for BG 100-180 mg/dL for T1DM, 100-150 mg/dL for T2DM. For cardiac surgery, target BG 100-150 mg/dL intra-op.
4 If T2DM pt on large doses @home, may require more insulin.
Pre-op: Day of surgery ✓BG q1-2h. ✓A1c1,2 (w/in last 60-90days). Target BG 100-180 mg/dL - ✓BG on arrival to pre-op. For hyperglycemia: If A1c reasonable (eg, stress hyperglycemia) OK for OR, after hyperglycemia controlled w/ correction insulin and BG monitoring q1-2h. If markedly high A1c: @ risk for impaired healing, consider deferring surgery until A1c1,2 closer to goal (eg, 8.5% or other goal)
- If high-risk pt (eg, txp or CABG), consider IM/endocrine consult
- Hold oral and noninsulin injectable antihyperglycemics (though research isn’t strong). Hold short-/rapid-acting insulins (unless BG >2003)
- Insulin regimen: If on home long-acting basal insulin, give 75%-100% of basal dose; for intermediate-acting and fixed-combo insulins, give 50%-75% of usual dose (50%-67% for NPH)
- For short procedure: Use SC insulin; may continue insulin pump4 use (eg, for T1DM or pregnant pts)
- For long procedure requiring prolonged NPO: Use IV insulin drip. If T1DM or T2DM on insulin as outpt, use insulin drip maintained @ 1-2 units/h5 w/ D5W at 50-75 cc/h, to maintain BG target3
- Treat hyperglycemia w/ IV or SC insulin; specify plan for hypoglycemia (<70 mg/dL)
Intra-op: ✓BG q1-2h; target BG 100-180 mg/dL (100-150 for intra-op cardiac surgery) - ✓BG: prior to anesthesia induction or incision, upon awakening, and on transfer to post-op. For longer surgeries, ✓BG q1h, esp if on insulin drip
- If hyper/hypoglycemia6 tx required, ✓BG frequently, eg, q15min
Footnotes 1 New hyperglycemia. Manage based on A1c level:
• 5.7%-6.4% Pre-diabetes. Lifestyle change; if multiple risk factors, consider metformin or other drugs
• 6.4%-7.4% Newly dx DM. Lifestyle + metformin
• 7.5%-9.0% Newly dx DM, uncontrolled. Lifestyle + mono- or dual-therapy
• 9%-10% Newly dx DM, uncontrolled. Lifestyle + double- or triple-therapy
• 10% Newly dx DM, uncontrolled. Lifestyle + metformin + basal/nutritional insulin preferred, esp if symptomatic; after glucose toxicity resolve, may transition to PO drugs
2 Known DM. Manage based on A1c level:
• <5.7%: Assess any pre-admit hypoglycemia; de-escalate home regimen if needed
• 5.7%-7.4% Controlled DM
• 7.5%-9.0% Uncontrolled DM. Lifestyle + dual-therapy
• 9%-10% Uncontrolled DM. Lifestyle + triple-therapy
• 10% Uncontrolled DM. Lifestyle + metformin + basal/nutritional insulin preferred, esp if symptomatic; after glucose toxicity resolves, may transition to PO drugs
3 Short-acting insulin (eg, lispro, aspart, glulisine): If BG >200, then use small doses (eg, 1-4 units) aiming for BG 100-180 mg/dL for T1DM, 100-150 mg/dL for T2DM. For cardiac surgery, target BG 100-150 mg/dL intra-op.
4 If undergoing surgery w/ anesthesia time <1h, some anesthesiologists will accept keeping pump running. If pump tx interrupted for >1h, insulin drip or SC basal/bolus insulin must be used.
5 If T2DM pt on large doses @home, may require more insulin.
6 ADA defines hypoglycemia <70 mg/dL, severe hypoglycemia <40 mg/dL. Tx w/ 50 mL of D50 (equivalent to 25 g carbohydrate, which ↑ BG by 125 mg/dL). Hypoglycemic risk factors: advanced age, malnutrition/cachexia/low BMI, ESLD, ESRD, sepsis, CHF, multiorgan failure, advanced malignancy.
✓BG q1-2h post-op; BG target 100-180 mg/dL,1 avoid/tx hypoglycemia2 (BG <70 mg/dL) - ✓BG: upon arrival to post-op, and q1-2h (q1h if on insulin drip)
- Consider endocrine/IM consult for high-risk pts (txp, CABG)
- Control post-op N/V; promote oral intake when appropriate. Specify insulin adjustments if nutrition is started/interrupted
- Create transition plan to ICU/ward/home
- If on insulin drip, admitting to ICU/ward: Transition to scheduled SC insulin3 once stable,4 based on estimated totally daily insulin,3 distributing 50% to once-daily basal and 50% to nutritional. For most pts, allow several hours overlap5 before d/c insulin drip. Continuing insulin drip may be appropriate if uncontrolled hyperglycemia on steroids, on TPN, hyperglycemic crisis, L&D pts, or if going to ICU intubated, on mod-high IV pressors, or unable to take nutrition. Continue to ✓BG, adjust for changes in nutrition
- If d/c to home: Resume home antihyperglycemic regimen, if it was effective,6 or arrange f/u for new7/uncontrolled6 hyperglycemia. If on metformin and NL renal function, OK to resume 48h post-op. If on α-glucosidase inhibitor, resume only when meals resumed. If on GLP-1 agonist (exenatide), resume when eating normally
Footnotes 1 Including post-cardiovascular surgery. Joint Commission’s Surgical Care Improvement Project recommends target glucose <180 mg/dL during 18-24h window post-anesthesia.
2 ADA defines hypoglycemia <70 mg/dL, severe hypoglycemia <40 mg/dL. Tx w/ 50 mL of D50 (equivalent to 25 g carbohydrate, which ↑ BG by 125 mg/dL). Hypoglycemic risk factors: advanced age, malnutrition/cachexia/low body mass, ESLD, ESRD, sepsis, CHF, multiorgan failure, advanced malignancy.
3 Scheduled SC insulin (applies to pts w/ known DM or new hyperglycemia on infusion rates >1-2 units/h): average the infusion rate over last 6-8h to estimate a 24-hr requirement (total daily dose). Reduce this by 20% to account for expected reduction in requirements. If eating, on tube feeds, or on TPN at transition time, divide total daily dose into 50% basal once daily, and 50% nutritional divided equally for meals/feeds. Adjust daily as needed.
4 Stable: no IV vasoconstrictor infusion, BG stable in target range, extubated, able to tolerate meal/other nutritional intake.
5 Overlap SC insulin with insulin drip. Several methods to overlap insulin infusion w/ basal insulin exist:
• Give 1st dose basal SC insulin 2-3h before infusion stopped, or
• Stop infusion, give 10% basal dose as rapid-acting along w/ basal insulin dose, or
• Give a dose of short- or rapid-acting insulin 1-2h before infusion stopped
6 Known DM. Managed based on A1c level:
• <5.7%: Assess any pre-admit hypoglycemia; de-escalate home regimen if needed
• 5.7%-7.4% Controlled DM
• 7.5%-9.0% Uncontrolled DM. Lifestyle + dual-therapy
• 9%-10% Uncontrolled DM. Lifestyle + triple-therapy
• 10% Uncontrolled DM. Lifestyle + metformin + basal/nutritional insulin preferred, esp if symptomatic; after glucose toxicity resolves, may transition to PO drugs
7 New hyperglycemia. Managed based on A1c level:
• 5.7%-6.4% Pre-diabetes. Lifestyle change; if multiple risk factors, consider metformin or other drugs
• 6.4%-7.4% Newly dx DM. Lifestyle + metformin
• 7.5%-9.0% Newly dx DM, uncontrolled. Lifestyle + mono- or dual-therapy
• 9%-10% Newly dx DM, uncontrolled. Lifestyle + double- or triple-therapy
• 10% Newly dx DM, uncontrolled. Lifestyle + metformin + basal/nutritional insulin preferred, esp if symptomatic; after glucose toxicity resolve, may transition to PO drugs
|