-
Presenting w/ insomnia, awaiting eval
Diagnose1 insomnia by clinical eval, incl hx, exam; consider DDx; identify comorbid conditions - Hx: sleep hx,1 PMHx, psych hx, substance use hx (eg, alcohol/caffeine/nicotine/illegal drugs)1,2
- Exam: PE and mental status1,2
- Epworth Sleepiness Scale, Insomnia Severity Index or other insomnia scale to identify sleepy pts/comorbid disorders,1-3 assist w/ baseline eval/outcomes f/u1
- Assign 2-wk sleep log to identify sleep-wake times, general patterns, and day-to-day variability1,2,4
- If sleep breathing (eg, OSA) or movement (eg, RLS) disorders suspected: order polysomnography2 (otherwise not routinely1,4); consider also when initial dx is uncertain,1 when sudden arousals occur w/ violent/injurious behavior,1 for at-risk occupations (eg, professional drivers),2 and when significant sleep-state misperception suspected2
- If circadian rhythm disturbance (incl depression-assoc insomnia) suspected: consider actigraphy1
- Polysomnography, multiple sleep latency testing not indicated for routine eval of chronic insomnia1,3
Common contributing meds and substances include:1,2 - Antidepressants (SSRIs, SNRIs, MAOIs)
- Stimulants (caffeine, methylphenidate, amphetamine derivatives, ephedrine and derivatives, cocaine)
- Alcohol, nicotine
- Decongestants (pseudoephedrine, phenylephrine, phenylpropanolamine)
- Narcotic analgesics (oxycodone, codeine, propoxyphene)
- Illegal drugs
- CV (β-blockers, α-receptor agonists and antagonists, diuretics, lipid-lowering agents)
- Pulmonary (theophylline, albuterol)
Consider DDx;1 use general medical/psych/medication questionnaire to help identify comorbid conditions: - If comorbidities (neuro, psych, fatigue): Use clinical judgment to decide whether to treat insomnia or comorbid condition first, or both concurrently2
- Assess for treatable secondary causes of insomnia such as depression, pain; BPH, substance abuse disorders, and other sleep disorders (OSA, RLS) before recommending that pts initiate/continue insomnia meds5
Footnotes 1 AASM 2008. Insomnia dx requires associated daytime dysfunction plus appropriate insomnia sx (ICSD-2 definition). ICSD-2 lists specific insomnia disorders w/ key features as follows: • Adjustment (Acute) Insomnia – insomnia assoc w/ identifiable stressor; short duration
• Psychophysiological Insomnia – heightened arousal or habitual sleep-preventing associations
• Paradoxical Insomnia – complaint of severe or almost complete insomnia that overestimates objective evidence of sleep disturbance
• Idiopathic Insomnia – persistent insomnia; insidious onset in early childhood; few or no remissions
• Insomnia d/t Mental Disorder – occurs only during mental disorder/triggered by that disorder
• Inadequate Sleep Hygiene – insomnia assoc w/ sleep practices/activities inconsistent w/ good sleep quality and daytime alertness
• Insomnia d/t Drug or Substance – sleep disruption d/t prescribed meds, recreational drug, caffeine, alcohol, food, or environmental toxin
• Insomnia d/t Medical Condition – insomnia resulting from/depending upon coexisting medical disorder or other physiological factor; features marked distress; warrants separate clinical attention
• Insomnia not d/t Substance/Known Physiological Condition, Unspecified and Physiologic (Organic) Insomnia, Unspecified – Used when further eval needed to identify specific assoc conditions, or when pt fails to meet criteria for more specific disorder
• Diagnose by clinical eval via thorough sleep hx and detailed medical, substance, and psychiatric hx [R3]. Sleep hx should cover specific insomnia complaints, presleep conditions, sleep-wake patterns, other sleep-related sx, and daytime consequences [R5].
• Physical and mental status exam may provide important info re: comorbid conditions and DDx [R3].
• Neither polysomnography nor daytime multiple sleep latency testing indicated in routine eval of chronic insomnia, incl insomnia d/t psych or neuropsych disorders [R3].
• Consider additional assessments for baseline/tx outcomes [R5].
• Differential: Presence of 1 insomnia disorder doesn't exclude other disorders; >1 primary/comorbid insomnia disorders may be present at the same time [R5].
Schutte-Rodin S, et al. Clinical Guideline for the Evaluation and Management of Chronic Insomnia in Adults. J Clin Sleep Med. 2008;4(5):487-504.
PDF at PubMed®Central
2 ESRS 2017.
• Recommend pts keep sleep diary for 7-14 days [R9].
• Use Insomnia Severity Index (ISI) to assess severity and to diagnose.
• Use Pittsburgh Sleep Quality Index (PSQI) to assess subjective sleep during previous mo, but not to diagnose insomnia.
• If suspect irregular sleep-wake schedules or circadian rhythm disorders: Order actigraphy [R9]; also consider for assessing quantitative sleep parameters [R10].
Riemann D, et al. European Guideline for the Diagnosis and Treatment of Insomnia. J Sleep Res. 2017 Dec;26(6):675-700. PDF
3 VA/DoD 2019. VA/DoD Clinical Practice Guideline for the Management of Chronic Insomnia Disorder and Obstructive Sleep Apnea. Version 1.0 – 2019. PDF
4 ACP 2016.
• In general, insomnia disorder is treated by clinicians on basis of pt-reported sleep-associated distress, not lab assessment.
• Polysomnography isn't indicated for dx or tx of insomnia disorder.
Wilt TJ, et al. Pharmacologic Treatment of Insomnia Disorder: An Evidence Report for a Clinical Practice Guideline by the American College of Physicians. Ann Intern Med. 2016;165(2):103-112. PubMed® abstract
5 ACP 2016. Qaseem A, et al. Management of Chronic Insomnia Disorder in Adults: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2016;165(2):125-33. PDF accessed online March 16, 2018
-
Candidate for multimodal CBT-I, s/p eval
Offer CBT-I1 as 1st-line tx for chronic insomnia1,2 in adults of any age;1-3multimodal CBT-I (administered by trained clinician/mental health professional) consists of the following:1 - Educational interventions (sleep hygiene); not alone, in absence of CBT-I, per VA4
- Behavioral strategies (sleep restriction,1 sleep diaries,3 stimulus control1,3)
- Relaxation training1,3
- Cognitive tx around sleep2,4,5
In select cases, may consider pharmaco-tx as temporary adjunct to CBT-I;2 combined tx (CBT-I + medication) no better/worse vs CBT-I alone; use depends on individualized factors5 If comorbidities: Use clinical judgment to decide whether to treat insomnia or comorbid condition first, or both concurrently3 Footnotes 1 ACP 2016.
• CBT-I is first-line tx [R7] [E6]. CBT-I likely to have fewer harms, whereas pharmaco-tx can be assoc w/ serious adverse events. Delivery methods include in-person individual or group tx, telephone- or Web-based modules, self-help books.
• Chronic insomnia is diagnosed per DSM-5 and International Classification of Sleep Disorders, which have similar dx criteria. Sx must cause clinically significant functional distress or impairment; be present at least 3 nights/wk at least 3mo; and not be linked to other sleep, medical, or mental disorders.
• Sleep restriction. Behavioral intervention that limits time in bed to sleep time, gradually increasing time spent in bed as sleep efficiency improves.
• Stimulus control. Behavioral tx to create consistency in sleep patterns and re-associate bed/bedroom w/ sleep (eg, only go to sleep when tired).
• Relaxation training. Training to reduce somatic tension and control bedtime thought patterns that impair sleep.
Qaseem A, et al. Management of Chronic Insomnia Disorder in Adults: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2016;165(2):125-33.
PDF accessed online March 16, 2018
2 AASM 2017.
• Chronic insomnia. AASM uses the International Classification of Sleep Disorders, Third Edition definition: A complaint of trouble initiating or maintaining sleep which is assoc w/ daytime consequences and isn’t attributable to environmental circumstance or inadequate opportunity to sleep. Chronic: persisting at least 3mo, at least 3x/wk.
• CBT-I. Previous AASM guidelines on eval and tx of chronic insomnia assert CBT-I to be the standard tx, w/ a significantly favorable benefit:risk ratio.
Sateia MJ, et al. Clinical Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017;13(2):307-349. PDF at PubMed®Central
3 ESRS 2017.
• CBT-I is first-line tx [R9] [E9]. Although CBT-I and hypnotics have comparable short-term efficacy, studies have shown CBT-I to be superior in the long-term. CBT-I also had good effects on comorbid conditions (anxiety, depression, PTSD, cancer, chronic pain).
• Sleep restriction curtails time in bed to actual amount of sleep being achieved. For example, if pt w/ insomnia reports sleeping 6.5h/night on average, initial recommended time in bed is restricted to 6.5h, w/ min sleep window of 4-6h advised, even when average sleep time is less. Weekly sleep window adjustments are made until optimal sleep duration reached.
• Strongly recommend use of sleep diaries to estimate sleep time, both before starting sleep restriction tx and also during f/u [R9].
• Stimulus control tx consists of behavioral instructions designed to re-associate bed/bedroom w/ sleep and re-establish consistent sleep-wake schedule:
1) Go to bed only when sleepy
2) Get out of bed when unable to sleep
3) Use bed/bedroom only for sleep/sex (eg, no reading, no watching TV)
4) Wake at same time very morning
5) Don’t nap during the day
• Relaxation tx includes clinical procedures to reduce somatic tension (eg, progressive muscle relaxation, autogenic training) or to reduce intrusive thoughts at bedtime (eg, imagery training, meditation).
• Cognitive strategies are psychological methods designed to change misconceptions/excessive concerns about sleep and insomnia and its perceived daytime consequences.
Riemann D, et al. European Guideline for the Diagnosis and Treatment of Insomnia. J Sleep Res. 2017 Dec;26(6):675-700. PDF
4 VA/DoD 2019. VA/DoD Clinical Practice Guideline for the Management of Chronic Insomnia Disorder and Obstructive Sleep Apnea. Version 1.0 – 2019. PDF
5 AASM 2008. Common cognitive distortions identified and addressed during tx include:
• “I can’t sleep without medication.”
• “I have a chemical imbalance.”
• “If I can’t sleep I should stay in bed and rest.”
• “My life will be ruined if I can’t sleep.”
If considering combined tx (CBT-I + meds): Take into account sx, tx goals, past tx responses, pt preference, cost, availability of other tx, comorbidities, contraindications, med interactions, and SEs [R5]. Combined tx not better/worse vs CBT-I alone; no comparative long-term pharmaco-tx studies available [R5].
Schutte-Rodin S, et al. Clinical Guideline for the Evaluation and Management of Chronic Insomnia in Adults. J Clin Sleep Med. 2008;4(5):487-504. PDF at PubMed®Central
-
CBT-I unavailable/inadequate, s/p eval
Use shared decision-making approach re: pharmaco-tx1 - Consider pharmacological tx only for short-term use1,2—ideally no longer than 4-5wk
- If insomnia doesn’t remit w/in 7-10 days of tx: Evaluate further. If shared decision made to continue meds ≥4-5wk: Reassess need for med continuation at periodic intervals1
- Reduce doses of BZD and nonBZD hypnotics in women, older, and/or debilitated adults;1 ESRS says to strongly consider reducing to intermittent dosing in pts taking daily BZDs, BZRAs, or sedating antidepressants2
- Harms of hypnotic agents include:1 cognitive/behavioral changes such as daytime impairment, “sleep driving,” worsening depression, suicidal thoughts/actions (primarily in depressed pts) and/or if taking both sedatives and hypnotics;3 may be assoc w/ infrequent, but serious harms (dementia, serious injury, increased risk for falls/hip fx/mobility problems in older adults)1,3
- Sedatives/hypnotics generally not recommended during pregnancy or lactation4
- Monitor tx response in older adults closely, as they may be more sensitive to meds and their adverse effects1
- Light tx/exercise may be useful as adjunct tx, but more studies needed2
- If behavioral/pharmacologic tx fails, or if reasonable suspicion of sleep breathing/movement disorder: Order polysomnography2,4
Suggested/proven pharmacological tx options:3,5 Not recommended: - sedating antidepressants for long-term tx of insomnia2
- antihistamines2 (incl diphenhydramine5)
- antipsychotics2
- tiagabine5
- trazodone5
- L-tryptophan (α-amino acid)5
- melatonin2,5
- valerian5 (and other phytotherapeutics2)
- complementary/alt tx2 (eg, homeopathy, yoga), although VA suggests offering auricular acupuncture6
Footnotes 1 ACP 2016. Use shared decision-making approach re: pharmaco-tx [R8] [E7].
Harms for BZDs:
• Daytime drowsiness, dizziness or lightheadedness, dementia
• Increased risk for falls, hip fractures, and mobility problems for older adults
• temazepam assoc w/ an increase in incident CA cases
Harms for non-BZDs:
• eszopiclone: somnolence, unpleasant taste, myalgia, memory impairment, psych-related adverse effects, depression, anxiety, accidental injury
• zaleplon: pain, somnolence or dizziness, GI events, arrhythmia, hallucinations
• zolpidem: anxiety, somnolence, altered mood, hallucinations, depression, psych-related adverse events, memory and driving impairment, risk for fx or major head injury or fx requiring hospitalization, increase in incident CA
• suvorexant: somnolence, cognitive and behavioral changes (eg, amnesia, anxiety, hallucinations, other neuropsych sx); complex behaviors (eg, “sleep driving”); worsening of depression, incl suicidal thinking in people w/ depression; daytime impairments; sleep paralysis; hypnagogic/hypnopompic hallucinations
• ramelteon: dizziness; somnolence (similar to placebo); fatigue; HA; unpleasant taste; nausea; new cognitive/behavioral abnormalities; complex behaviors (eg, “sleep driving”); exacerbation of depression and suicidal ideation (primarily in depressed pts)
• doxepin: sedation, fatigue, weakness, lethargy, dry mouth, constipation, blurred vision, HA
Qaseem A, et al. Management of Chronic Insomnia Disorder in Adults: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2016;165(2):125-33. PubMed® abstract
2 ESRS 2017.
Short-term impact of pharmaco-tx:
• BZDs, BZRAs, and some sedating antidepressants are effective for short-term (≤4wks) tx [E9]
• Newer BZRAs are equally effective as BZDs [E10]
• BZDs/BZRAs w/ shorter half-lives may have fewer side effects re: sedation in morning [E10]
Long-term impact of pharmaco-tx:
• BZDs or BZRAs not recommended for longer-term tx, d/t lack of evidence and possible SEs/risks [R9] [E11]
• In pts using these meds daily, reducing to intermittent dosing is strongly recommended [R9] [E11]
• Sedating antidepressants effective in short-term tx; carefully consider contraindications [E10]
Not recommended for tx of insomnia:
• sedating antidepressants for long-term tx, d/t lack of evidence and possible SEs/risks [R9] [E11]
• antihistamines, d/t insufficient evidence [R9] [E11]
• antipsychotics, d/t insufficient evidence/SEs [R9] [E12]
• melatonin, d/t low efficacy [R10] [E11]
• valerian and other phytotherapeutics, d/t poor evidence [R10] [E11]
• complementary/alt tx (eg, acupuncture, aromatherapy, foot reflexology, homeopathy, meditative movement, moxibustion, and yoga) tx d/t poor evidence [R10] [E12]
Light tx/exercise may be useful as adjunct tx, but more studies needed [R10] [E11].
Riemann D, et al. European Guideline for the Diagnosis and Treatment of Insomnia. J Sleep Res. 2017 Dec;26(6):675-700. PDF
3 ACP 2016.
• Sleep driving=driving after taking a hypnotic but having no recollection of driving.
• Harms. Observational studies, incl FDA data, suggest an assoc btwn hypnotics w/ infrequent, but serious harms.
• Dose reduction advised in women and older/debilitated adults; drugs taken at bedtime remain at levels high enough to interfere w/ morning driving.
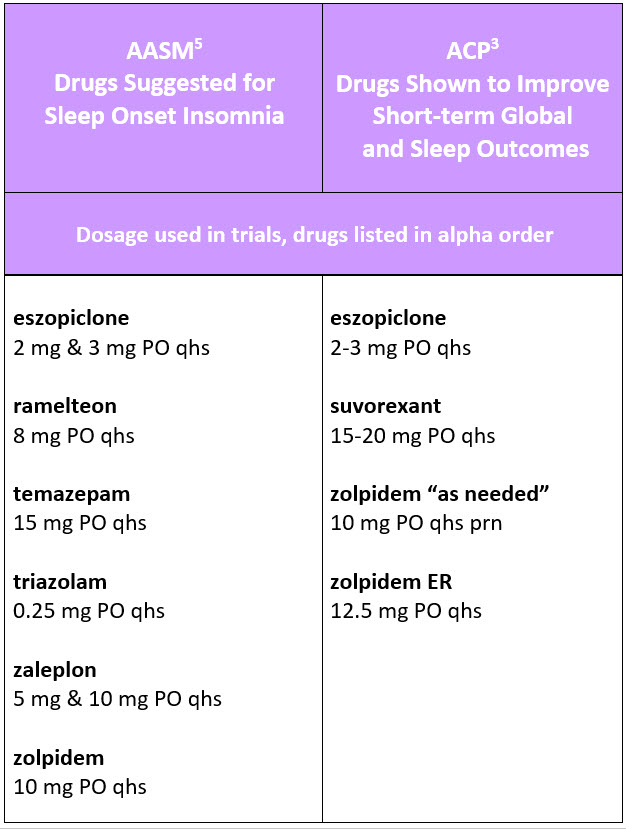
Drugs shown to improve short-term global and sleep outcomes:
• eszopiclone (trials used 2-3 mg PO qhs) [E6]
• suvorexant (trials used 15-20 mg PO qhs) [E6]
• zolpidem “as needed” (trials used 10 mg PO qhs prn) [E6]
• zolpidem ER (trials used 12.5 mg PO qhs) [E7]
Eszopiclone, zolpidem, and suvorexant improved short-term outcomes (eg, Insomnia Severity Index scores, sleep onset latency, total sleep time, wake time after sleep onset) vs placebo in small, limited-duration trials. Nonetheless, absolute effect sizes were small; in some cases, researchers noted adverse events.
Wilt TJ, et al. Pharmacologic Treatment of Insomnia Disorder: An Evidence Report for a Clinical Practice Guideline by the American College of Physicians. Ann Intern Med. 2016;165(2):103-112. PubMed® abstract
4 AASM 2008. Schutte-Rodin S, et al. Clinical Guideline for the Evaluation and Management of Chronic Insomnia in Adults. J Clin Sleep Med. 2008;4(5):487-504. PDF at PubMed®Central
5 AASM 2017.
Suggested for treating sleep onset insomnia:
• eszopiclone (mean reduction in sleep latency 14min greater than placebo; trials used 2 mg and 3 mg PO qhs) [R2] [E4]
• ramelteon (mean reduction in sleep latency 9min greater than placebo; trials used 8 mg PO qhs) [R2] [E4]
• temazepam (mean reduction in sleep latency 37min greater than placebo; trials used 15 mg PO qhs) [R2] [E2]
• triazolam (mean reduction in sleep latency 9min greater than placebo; trials used 0.25 mg PO qhs) [R2] [E1]
• zaleplon (mean reduction in sleep latency 10min greater than placebo; trials used 5 mg and 10 mg PO qhs) [R2] [E3]
• zolpidem (mean reduction in sleep latency 5-12min greater than placebo; trials used 10 mg PO qhs) [R2] [E4]
Not recommended for tx of either sleep onset or sleep maintenance insomnia in adults:
• diphenhydramine (antihistamine) [R2]
• tiagabine (anticonvulsant) [R2]
• trazodone (antidepressant) [R2]
• L-tryptophan (α-amino acid) [R2]
• melatonin, d/t low efficacy [R2]
• valerian [R2]
Sateia MJ, et al. Clinical Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017;13(2):307-349. PDF
6 VA/DoD 2019. VA/DoD Clinical Practice Guideline for the Management of Chronic Insomnia Disorder and Obstructive Sleep Apnea. Version 1.0 – 2019. PDF Sleep maintenance insomnia Use shared decision-making approach re: pharmaco-tx1 - Consider pharmacological tx only for short-term use1,2—ideally no longer than 4-5wk
- If insomnia doesn’t remit w/in 7-10 days of tx: Evaluate further. If shared decision made to continue meds ≥4-5wk: Reassess need for med continuation at periodic intervals1
- Reduce doses of BZD and non-BZD hypnotics in women, older, and/or debilitated adults;1 ESRS says to strongly consider reducing to intermittent dosing in pts taking daily BZDs, BZRAs, or sedating antidepressants2
- Harms of hypnotic agents include:1 cognitive/behavioral changes such as daytime impairment, “sleep driving,” worsening depression, suicidal thoughts/actions (primarily in depressed pts)1 and/or if taking both sedatives and hypnotics;3) may be assoc w/ infrequent, but serious harms (dementia, serious injury, increased risk for falls/hip fx/mobility problems in older adults)1,3
- Sedatives/hypnotics generally not recommended during pregnancy or lactation4
- Monitor tx response in older adults closely, as they may be more sensitive to meds and their adverse effects1
- Light tx/exercise may be useful as adjunct tx, but more studies needed2
- If behavioral/pharmacologic tx fails, or if reasonable suspicion of sleep breathing/movement disorder: Order polysomnography2,4
Suggested/proven pharmacological tx options:3,5 Not recommended: - sedating antidepressants for long-term tx of insomnia2
- antihistamines2 (incl diphenhydramine5)
- antipsychotics2
- tiagabine5
- trazodone5
- L-tryptophan (α-amino acid)5
- melatonin2,5
- valerian5 (and other phytotherapeutics2)
- complementary/alt tx2 (eg, acupuncture, homeopathy, yoga)
Footnotes 1 ACP 2016. Use shared decision-making approach re: pharmaco-tx [R8] [E7].
Harms for BZDs:
• Daytime drowsiness, dizziness or lightheadedness, dementia
• Increased risk for falls, hip fractures, and mobility problems for older adults
• temazepam assoc w/ an increase in incident CA cases
Harms for non-BZDs:
• eszopiclone: somnolence, unpleasant taste, myalgia, memory impairment, psych-related adverse effects, depression, anxiety, accidental injury
• zolpidem: anxiety, somnolence, altered mood, hallucinations, depression, psych-related adverse events, memory and driving impairment, risk for fx or major head injury or fx requiring hospitalization, increase in incident CA
• suvorexant: somnolence, cognitive and behavioral changes (eg, amnesia, anxiety, hallucinations, other neuropsych sx); complex behaviors (eg, “sleep driving”); worsening of depression, incl suicidal thinking in people w/ depression; daytime impairments; sleep paralysis; hypnagogic/hypnopompic hallucinations
• doxepin: sedation, fatigue, weakness, lethargy, dry mouth, constipation, blurred vision, HA
Qaseem A, et al. Management of Chronic Insomnia Disorder in Adults: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2016;165(2):125-33. PubMed® abstract
2 ESRS 2017.
Short-term impact of pharmaco-tx:
• BZDs, BZRAs, and some sedating antidepressants are effective for short-term (≤4wks) tx [E9]
• Newer BZRAs are equally effective as BZDs [E10]
• BZDs/BZRAs w/ shorter half-lives may have less side-effects re: sedation in morning [E10]
Long-term impact of pharmaco-tx:
• BZDs or BZRAs not recommended for longer-term tx d/t lack of evidence and possible SEs/risks [R9] [E11]
• In pts using these meds daily, reducing to intermittent dosing is strongly recommended [R9] [E11]
• Sedating antidepressants effective in short-term tx; carefully consider contraindications [E10]
Not recommended for treatment of insomnia:
• sedating antidepressants for long-term tx, d/t lack of evidence and possible SEs/risks [R9] [E11]
• antihistamines, d/t insufficient evidence [R9] [E11]
• antipsychotics, d/t insufficient evidence/SEs [R9] [E12]
• melatonin, d/t low efficacy [R10] [E11]
• valerian and other phytotherapeutics, d/t poor evidence [R10] [E11]
• complementary/alt tx (eg, acupuncture, aromatherapy, foot reflexology, homeopathy, meditative movement, moxibustion, and yoga) tx d/t poor evidence [R10] [E12]
Light tx/exercise may be useful as adjunct tx, but more studies needed [R10] [E11].
Riemann D, et al. European Guideline for the Diagnosis and Treatment of Insomnia. J Sleep Res. 2017 Dec;26(6):675-700. PDF
3 ACP 2016.
• Sleep driving=driving after taking a hypnotic but having no recollection of driving.
• Harms. Observational studies, incl FDA data, suggest an assoc btwn hypnotics w/ infrequent, but serious harms.
• Dose reduction advised in women and older/debilitated adults; drugs taken at bedtime remain at levels high enough to interfere w/ morning driving.
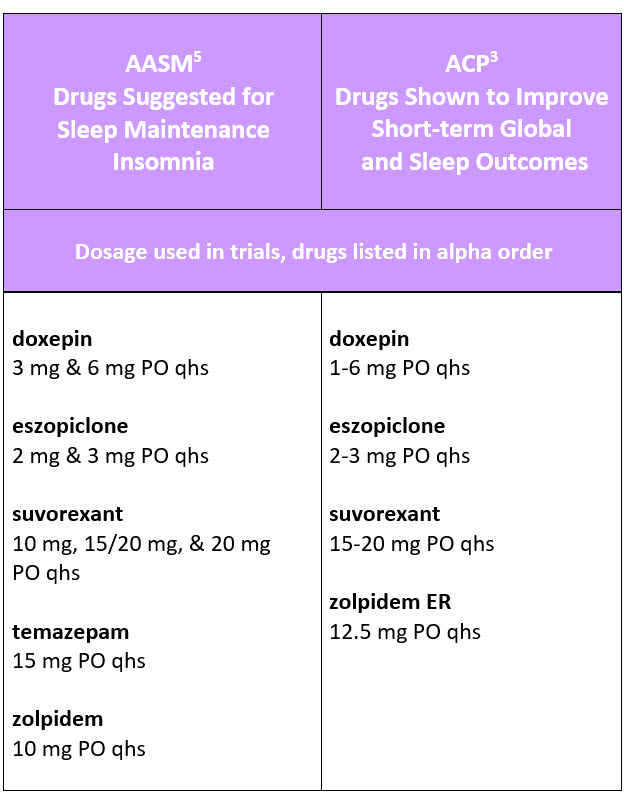
Drugs shown to improve short-term global and sleep outcomes:
• doxepin (trials used 1-6 mg PO qhs) [E7]
• eszopiclone (trials used 2-3 mg PO qhs) [E7]
• suvorexant (trials used 15-20 mg PO qhs) [E6]
• zolpidem ER (trials used 12.5 mg PO qhs) [E7]
Eszopiclone, zolpidem, and suvorexant improved short-term outcomes (eg, Insomnia Severity Index scores, sleep onset latency, total sleep time, wake-time after sleep onset) vs placebo in small, limited-duration trials. Nonetheless, absolute effect sizes were small; in some cases, researchers noted adverse events.
Wilt TJ, et al. Pharmacologic Treatment of Insomnia Disorder: An Evidence Report for a Clinical Practice Guideline by the American College of Physicians. Ann Intern Med. 2016;165(2):103-112. PubMed® abstract
4 AASM 2008. Schutte-Rodin S, et al. Clinical Guideline for the Evaluation and Management of Chronic Insomnia in Adults. J Clin Sleep Med. 2008;4(5):487-504. PDF at PubMed®Central
5 AASM 2017.
Suggested for treating sleep maintenance insomnia:
• doxepin (total sleep time improved by a mean of 26-32min vs placebo; trials used 3 mg and 6 mg PO qhs) [R2] [E3]
• eszopiclone (total sleep time improved by a mean of 28-57min vs placebo; trials used 2 mg and 3 mg PO qhs) [R2] [E4]
• suvorexant (total sleep time improved by a mean of 10min vs placebo; trials used 10 mg, 15/20 mg, and 20 mg PO qhs) [R2] [E3]
• temazepam (total sleep time improved by a mean of 99min vs placebo; trials used 15 mg PO qhs) [R2] [E2]
• zolpidem (total sleep time improved by a mean of 29min vs placebo; trials used 10 mg PO qhs) [R2] [E4]
Not recommended for treatment of either sleep onset or sleep maintenance insomnia in adults:
• diphenhydramine (antihistamine) [R2]
• tiagabine (anticonvulsant) [R2]
• trazodone (antidepressant) [R2]
• L-tryptophan (α-amino acid) [R2]
• melatonin, d/t low efficacy [R2]
• valerian [R2]
Sateia MJ, et al. Clinical Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017;13(2):307-349. PDF
|