-
Pt w/ typical Lyme sx (erythema migrans, carditis, arthritis, neuro sx, acrodermatitis chronica atrophicans)
Needs dx and/or initial tx Pt w/ early localized Lyme sx (erythema migrans) Diagnose & treat based on clinical finding of typical erythema migrans (EM) lesion; testing necessary only if skin findings suggestive of EM, but not typical - Treat empirically w/ PO doxycycline or amoxicillin;1-3 cefuroxime axetil also a 1st-line option1,2,*
- If pt unable to take doxycycline or beta-lactams, use azithromycin as 2nd-line choice,4 but monitor closely for response1
CDC 2022 & IDSA/AAN/ACR: Recommended abx dosing/duration for EM1,2 NICE 2018: Recommended abx dosing/duration for EM3 Consider testing in select circumstances; treat for Lyme w/o testing in pts w/ possible STARI in areas where Lyme is endemic - Assess for anaplasmosis and/or babesiosis in pts w/ high fever or characteristic lab abnormalities in areas where these infxns are endemic5
- If EM-like rash in area where Lyme and STARI are endemic and tick not ID’d, treat for Lyme w/o testing2
- In pts w/ potential tick exposure in a Lyme dz–endemic area who have 1+ skin lesions suggestive of, but atypical for, EM, consider Ab testing performed on acute-phase serum sample, followed by convalescent-phase serum sample (2-3wk later) if initial result is (-)2
- Don’t use unaccredited labs or unvalidated tests for Lyme dx3,6
Footnotes 1 CDC 2022. Lyme Disease: Erythema migrans rash. Last reviewed 3/1/22. Accessed 6/20/23
2 IDSA/AAN/ACR 2020. Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
3 NICE 2018. Lyme Disease - NICE Guideline (NG95). National Institute for Health and Care Excellence. Published 4/11/18. Last updated 10/17/18. Accessed 5/31/23
4 IDSA/AAN/ACR 2020. Use azithromycin as 2nd-line agent in pts w/ contraindications to all others; concern about ↓efficacy and macrolide resistance
• azithromycin 500 mg (10 mg/kg/dose, up to max 500 mg in children) PO qd – 5-10 days (7 days pref’d in U.S.)
Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
5 IDSA/AAN/ACR 2020. Characteristic lab abnormalities in both anaplasmosis & babesiosis incl:
• thrombocytopenia
• leukopenia
• neutropenia
• anemia
Evidence of hemolysis (anemia, ↑indirect bili, ↑LDH) particularly suggestive of babesiosis.
Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
6 CDC 2023. Examples of unvalidated tests include:
• Capture assays for antigens in urine
• Immunofluorescence staining, or cell sorting of cell wall–deficient or cystic forms of B burgdorferi
• Lymphocyte transformation tests
• Quantitative CD57 lymphocyte assays
• “Reverse Western blots”
• In-house criteria for interpretation of FDA-cleared tests
• IgM or IgG tests w/o previous enzyme immunoassay
Lyme Disease: Laboratory tests and practices that are not currently recommended. Last reviewed 2/9/23. Accessed 6/20/23
* ILADS 2014. ILADS diverges from CDC, IDSA, & NICE, recommending extended tx of at least 4-6wk w/ doxycycline, amoxicillin, or cefuroxime axetil. They also recommend that azithromycin be used for a minimum of 21 days, and that, regardless of abx used, tx be extended indefinitely until all sx are completely resolved.
Cameron DJ, et al. Evidence Assessments and Guideline Recommendations in Lyme Disease: The Clinical Management of Known Tick Bites, Erythema migrans Rashes and Persistent Disease. Expert Rev Anti Infect Ther. 2014. Sept;12(9):1103-1135. Free full-text PDF @ PubMed® Central
Numerous groups, incl the Infectious Diseases Society of America (IDSA), have raised concern about the quality, validity, and inherent bias of International Lyme and Associated Diseases Society (ILADS) guidance, which does not meet epocrates editorial standards. We include their recommendations here not as an endorsement of their validity but to provide context when confronted w/ pt questions arising from ILADS recommendations.
Pt w/ early disseminated Lyme sx (inflammatory arthritis, meningitis, cranial neuritis, carditis) Use 2-tier serum Ab testing strategy - Perform 2-tier testing over PCR or cx of blood, CSF, or synovial fluid: initial ELISA1,2 or IFA,1 then Western immunoblot (or FDA-approved 2nd EIA3) if 1st test is (+) or equivocal;1 don’t r/o dx if tests are (-) but there’s high clinical suspicion of Lyme dz2
- If CSF testing is done, perform simultaneous serum sample for determination of CSF:serum Ab index; don’t perform CSF serology alone, or perform CSF PCR or cx4
- In seropositive pts w/ Lyme arthritis needing more definitive info for tx decisions, use PCR of synovial fluid or tissue (over cx)4
- Assess for anaplasmosis and/or babesiosis in pts w/ high fever or characteristic lab abnormalities in areas where these infxns are endemic5
- Don't screen w/ EKG; perform EKG only in pts w/ s/sx consistent w/ carditis (eg, dyspnea, palpitations, edema, chest pain, dizziness, syncope)4
- Don’t use unaccredited labs or unvalidated tests for Lyme dx2,6
Footnotes 1 CDC 2023. Lyme Disease: Laboratory tests and practices that are not currently recommended. Last reviewed 2/9/23. Accessed 6/20/23
2 NICE 2018. Lyme Disease - NICE Guideline (NG95). National Institute for Health and Care Excellence. Published 4/11/18. Last updated 10/17/18. Accessed 5/31/23
3 CDC 2019. Mead P, et al. Updated CDC Recommendation for Serologic Diagnosis of Lyme Disease. Morb Mortal Wkly Rep. 2019;68:703. PDF
4 IDSA/AAN/ACR 2020. Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
5 IDSA/AAN/ACR 2020. Characteristic lab abnormalities in both anaplasmosis and babesiosis include:
• thrombocytopenia
• leukopenia
• neutropenia
• anemia
Evidence of hemolysis (anemia, ↑indirect bili, ↑LDH) particularly suggestive of babesiosis.
Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
6 CDC 2023. Examples of unvalidated tests include:
• Capture assays for antigens in urine
• Immunofluorescence staining, or cell sorting of cell wall–deficient or cystic forms of B burgdorferi
• Lymphocyte transformation tests
• Quantitative CD57 lymphocyte assays
• “Reverse Western blots”
• In-house criteria for interpretation of FDA-cleared tests
• IgM or IgG tests w/o previous enzyme immunoassay
Lyme Disease: Laboratory tests and practices that are not currently recommended. Last reviewed 2/9/23. Accessed 6/20/23
Awaiting initial tx for Lyme arthritis Arthritis is most common presentation of early disseminated Lyme, may occur in ¼ of cases - Treat Lyme arthritis w/ PO abx initially: doxycycline or amoxicillin (28 days);1-3 cefuroxime axetil also a 1st-line option1,3,*
CDC 2021 & IDSA/AAN/ACR: Recommended abx dosing/duration for Lyme arthritis:1,3 NICE-recommended abx dosing/duration for Lyme arthritis:2 Footnotes 1 CDC 2021. Lyme Disease: Lyme arthritis. Last reviewed 10/7/21. Accessed 6/20/23
2 NICE 2018. Lyme Disease - NICE Guideline (NG95). National Institute for Health and Care Excellence. Published 4/11/18. Last updated 10/17/18. Accessed 5/31/23
3 IDSA/AAN/ACR 2020. Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
4 IDSA/AAN/ACR 2020. IDSA includes doxycycline as an option in children <8 yo, noting that “a growing consensus accepts the safety of doxycycline use children for at least up to 14-days duration, but more data on safety would be desirable.” Consider risks/benefits of other abx when deciding to use doxycycline.
Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
* ILADS 2021. ILADS diverges from CDC, IDSA, and NICE, recommending extended tx of at least 4-6wk w/ doxycycline, amoxicillin, or cefuroxime axetil for EM, and stating that pts w/ disseminated dz may need even longer courses & possibly combinations of multiple abx.
Lyme Disease Basics for Providers: A Brief Primer by International Lyme and Associated Diseases Society. Accessed 5/31/23
Numerous groups, incl the Infectious Diseases Society of America (IDSA), have raised concern about the quality, validity, and inherent bias of International Lyme and Associated Diseases Society (ILADS) guidance, which does not meet epocrates editorial standards. We include their recommendations here not as an endorsement of their validity but to provide context when confronted w/ pt questions arising from ILADS recommendations. Awaiting initial tx for neurologic Lyme (facial palsy, neuritis, meningitis, encephalitis) Abx choice & duration depend on presentation of neurologic Lyme; facial palsy is most common (9%), followed by radiculopathy (4%) & meningoencephalitis (3%)1 - For facial palsy, use PO doxycycline (14-21 days per IDSA & CDC, 21 days per NICE);1-3 IV ceftriaxone, cefotaxime, & penicillin G also options, per IDSA;3 PO amoxicillin an option, per NICE;2,* no recommendations re: steroids w/ abx for Lyme-assoc facial palsy, per IDSA3
- For radiculitis or other peripheral nervous system (PNS) sx, use PO doxycycline1-3 or IV ceftriaxone (14-21 days);1,3 IV cefotaxime & penicillin G are options, per IDSA;3 PO amoxicillin an option, per NICE2
- If encephalitis or parenchymal infxn of spinal cord, use IV abx, per IDSA;3 NICE favors parenteral abx, as well, but considers PO doxycycline as 1st alternative2
- If meningitis, use radiculitis & PNS abx choices, per CDC & IDSA;1,3 NICE guidance groups all CNS involvement together, favors IV abx2
CDC 2021 & IDSA/AAN/ACR: Recommended abx dosing/duration for Lyme-assoc facial palsy:1,3 NICE-recommended abx dosing/duration for Lyme involving cranial nerves or peripheral nervous system:2 CDC 2021 & IDSA/AAN/ACR: Recommended abx dosing/duration for Lyme-assoc meningitis or radiculoneuritis:1,3 NICE-recommended abx dosing/duration for Lyme involving CNS:2 Footnotes 1 CDC 2021. Lyme Disease: Neurologic Lyme Disease. Last reviewed 8/11/21. Accessed 6/20/23
2 NICE 2018. Lyme Disease - NICE Guideline (NG95). National Institute for Health and Care Excellence. Published 4/11/18. Last updated 10/17/18. Accessed 5/31/23
3 IDSA/AAN/ACR 2020. Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
* ILADS 2021. ILADS diverges from CDC, IDSA, and NICE, recommending extended tx of at least 4-6wk w/ doxycycline, amoxicillin, or cefuroxime axetil for EM, and stating that pts w/ disseminated dz may need even longer courses & possibly combinations of multiple abx.
Lyme Disease Basics for Providers: A Brief Primer by International Lyme and Associated Diseases Society. Accessed 5/31/23
Numerous groups, incl the Infectious Diseases Society of America (IDSA), have raised concern about the quality, validity, and inherent bias of International Lyme and Associated Diseases Society (ILADS) guidance, which does not meet epocrates editorial standards. We include their recommendations here not as an endorsement of their validity but to provide context when confronted w/ pt questions arising from ILADS recommendations.
Awaiting initial tx for Lyme carditis Mild/hemodynamically stable Mild carditis (1st-deg AVB w/ PR <300 ms)1 can be treated w/ PO doxycycline,1-3 amoxicillin, cefuroxime axetil,1,3 or azithromycin3,* CDC 2022 & IDSA/AAN/ACR: Recommended abx dosing/duration for mild Lyme carditis:1,3 NICE-recommended abx dosing/duration for hemodynamically stable Lyme carditis:2 Footnotes 1 CDC 2022. Lyme Disease: Lyme carditis. Last reviewed 2/24/22. Accessed 6/20/23
2 NICE 2018. Lyme Disease - NICE Guideline (NG95). National Institute for Health and Care Excellence. Published 4/11/18. Last updated 10/17/18. Accessed 5/31/23
3 IDSA/AAN/ACR 2020. Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
* ILADS 2021. ILADS diverges from CDC, IDSA, and NICE, recommending extended tx of at least 4-6wk w/ doxycycline, amoxicillin, or cefuroxime axetil for EM, and stating that pts w/ disseminated dz may need even longer courses & possibly combinations of multiple abx.
Lyme Disease Basics for Providers: A Brief Primer by International Lyme and Associated Diseases Society. Accessed 5/31/23
Numerous groups, incl the Infectious Diseases Society of America (IDSA), have raised concern about the quality, validity, and inherent bias of International Lyme and Associated Diseases Society (ILADS) guidance, which does not meet epocrates editorial standards. We include their recommendations here not as an endorsement of their validity but to provide context when confronted w/ pt questions arising from ILADS recommendations.
Severe/hemodynamically unstable Unstable or severe dz1,3 requires hospitalization & IV ceftriaxone;1-3 consider temporary pacemaker, if symptomatic bradycardia2
CDC 2022 & IDSA/AAN/ACR: Recommended abx dosing/duration for severe Lyme carditis:1,2 NICE-recommended abx dosing/duration for hemodynamically unstable Lyme carditis:3 Footnotes 1 CDC 2022. Severe carditis: symptomatic, 1st-deg AV block w/ PR interval ≥300 ms, 2nd- or 3rd-deg AV block
Lyme Disease: Lyme carditis. Last reviewed 2/24/22. Accessed 6/20/23
2 IDSA/AAN/ACR 2020. Severe carditis: PR interval >300 ms, other arrhythmias, exercise intolerance, palpitations, syncope/presyncope, pericardial pain or effusion, elevated biomarkers (eg, troponin), edema, dyspnea
Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
3 NICE 2018. Lyme Disease - NICE Guideline (NG95). National Institute for Health and Care Excellence. Published 4/11/18. Last updated 10/17/18. Accessed 5/31/23 Pt w/ late disseminated Lyme sx (chronic arthritis, acrodermatitis chronica atrophicans, encephalopathy, polyneuropathy) Use 2-tier serum Ab testing strategy - Perform 2-tier testing over PCR or cx of blood, CSF, or synovial fluid: initial ELISA1,2 or IFA,1 then Western immunoblot (or FDA-approved 2nd EIA3) if 1st test is (+) or equivocal;1 don’t r/o dx if tests are (-) but there’s high clinical suspicion of Lyme dz2
- If CSF testing is done, perform simultaneous serum sample for determination of CSF:serum Ab index; don’t perform CSF serology alone, or perform CSF PCR or cx4
- In seropositive pts w/ Lyme arthritis needing more definitive info for tx decisions, use PCR of synovial fluid or tissue (over cx)4
- Don’t use unaccredited labs or unvalidated tests for Lyme dx2,5
Footnotes 1 CDC 2023. Lyme Disease: Laboratory tests and practices that are not currently recommended. Last reviewed 2/9/23. Accessed 6/20/23
2 NICE 2018. Lyme Disease - NICE Guideline (NG95). National Institute for Health and Care Excellence. Published 4/11/18. Last updated 10/17/18. Accessed 5/31/23
3 CDC 2019. Mead P, et al. Updated CDC Recommendation for Serologic Diagnosis of Lyme Disease. Morb Mortal Wkly Rep. 2019;68:703. PDF
4 IDSA/AAN/ACR 2020. Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
5 CDC 2023. Examples of unvalidated tests include:
• Capture assays for antigens in urine
• Immunofluorescence staining, or cell sorting of cell wall–deficient or cystic forms of B burgdorferi
• Lymphocyte transformation tests
• Quantitative CD57 lymphocyte assays
• “Reverse Western blots”
• In-house criteria for interpretation of FDA-cleared tests
• IgM or IgG tests w/o previous enzyme immunoassay
Lyme Disease: Laboratory tests and practices that are not currently recommended. Last reviewed 2/9/23. Accessed 6/20/23
Awaiting initial tx for chronic Lyme arthritis Treat for arthritis in late disseminated dz; people who don’t receive prompt tx for Lyme arthritis are at risk of developing permanent joint damage1 - Treat Lyme arthritis w/ PO abx initially: doxycycline or amoxicillin (28 days);1-3 cefuroxime axetil also a 1st-line option1,3,*
CDC 2021 & IDSA/AAN/ACR: Recommended abx dosing/duration for Lyme arthritis:1,3 NICE-recommended abx dosing/duration for Lyme arthritis:2 Footnotes 1 CDC 2021. Lyme Disease: Lyme arthritis. Last reviewed 10/7/21. Accessed 6/20/23
2 NICE 2018. Lyme Disease - NICE Guideline (NG95). National Institute for Health and Care Excellence. Published 4/11/18. Last updated 10/17/18. Accessed 5/31/23
3 IDSA/AAN/ACR 2020. Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
* ILADS 2021. ILADS diverges from CDC, IDSA, and NICE, recommending extended tx of at least 4-6wk w/ doxycycline, amoxicillin, or cefuroxime axetil for EM, and stating that pts w/ disseminated dz may need even longer courses & possibly combinations of multiple abx.
Lyme Disease Basics for Providers: A Brief Primer by International Lyme and Associated Diseases Society. Accessed 5/31/23
Numerous groups, incl the Infectious Diseases Society of America (IDSA), have raised concern about the quality, validity, and inherent bias of International Lyme and Associated Diseases Society (ILADS) guidance, which does not meet epocrates editorial standards. We include their recommendations here not as an endorsement of their validity but to provide context when confronted w/ pt questions arising from ILADS recommendations. Awaiting initial tx for acrodermatitis chronica atrophicans Treat for acrodermatitis chronica atrophicans (ACA) in late disseminated dz; lesions treated early may fully resolve; however, pts w/ later-stage ACA may have permanent skin damage even after tx3 PNS involvement, esp sensory polyneuropathy, is common;3 varying degrees of permanent nervous system damage may develop in pts who don’t receive tx in early dz stages and who develop late-stage dz1 - Treat acrodermatitis chronica atrophicans w/ 21-28 days of PO abx2 (28 days, per NICE)3,*
IDSA/AAN/ACR: Recommended abx dosing/duration for acrodermatitis chronica atrophicans:2 NICE-recommended abx dosing/duration for acrodermatitis chronica atrophicans:2 Footnotes 1 CDC 2021. Lyme Disease: Neurologic Lyme Disease. Last reviewed 8/11/21. Accessed 6/20/23
2 NICE 2018. Lyme Disease - NICE Guideline (NG95). National Institute for Health and Care Excellence. Published 4/11/18. Last updated 10/17/18. Accessed 5/31/23
3 IDSA/AAN/ACR 2020. Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
* ILADS 2021. ILADS diverges from CDC, IDSA, and NICE, recommending extended tx of at least 4-6wk w/ doxycycline, amoxicillin, or cefuroxime axetil for EM, and stating that pts w/ disseminated dz may need even longer courses & possibly combinations of multiple abx.
Lyme Disease Basics for Providers: A Brief Primer by International Lyme and Associated Diseases Society. Accessed 5/31/23
Numerous groups, incl the Infectious Diseases Society of America (IDSA), have raised concern about the quality, validity, and inherent bias of International Lyme and Associated Diseases Society (ILADS) guidance, which does not meet epocrates editorial standards. We include their recommendations here not as an endorsement of their validity but to provide context when confronted w/ pt questions arising from ILADS recommendations. Awaiting initial tx for chronic encephalopathy/polyneuropathy Treat for neurologic Lyme in late disseminated dz; although most pts respond well to abx and fully recover, permanent nervous system damage may develop in those not treated in early dz stages and who develop late-stage dz1
- If encephalitis or parenchymal infxn of spinal cord, use IV abx, per IDSA;2 NICE favors parenteral abx, as well, but considers PO doxycycline as 1st alternative;3 use PO abx for peripheral nervous system sx3,*
IDSA/AAN/ACR: Recommended abx dosing/duration for Lyme encephalitis or parenchymal infxn of spinal cord:2 NICE-recommended abx dosing/duration for Lyme involving CNS:3 NICE-recommended abx dosing/duration for Lyme involving peripheral nervous system:3 Footnotes 1 CDC 2021. Lyme Disease: Neurologic Lyme Disease. Last reviewed 8/11/21. Accessed 6/20/23
2 IDSA/AAN/ACR 2020. Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
3 NICE 2018. Lyme Disease - NICE Guideline (NG95). National Institute for Health and Care Excellence. Published 4/11/18. Last updated 10/17/18. Accessed 5/31/23
* ILADS 2021. ILADS diverges from CDC, IDSA, and NICE, recommending extended tx of at least 4-6wk w/ doxycycline, amoxicillin, or cefuroxime axetil for EM, and stating that pts w/ disseminated dz may need even longer courses & possibly combinations of multiple abx.
Lyme Disease Basics for Providers: A Brief Primer by International Lyme and Associated Diseases Society. Accessed 5/31/23
Numerous groups, incl the Infectious Diseases Society of America (IDSA), have raised concern about the quality, validity, and inherent bias of International Lyme and Associated Diseases Society (ILADS) guidance, which does not meet epocrates editorial standards. We include their recommendations here not as an endorsement of their validity but to provide context when confronted w/ pt questions arising from ILADS recommendations. Pt w/ persistent sx after initial tx Lyme sx may persist for months after tx, but observe for objective signs of reinfxn or tx failure; consider concurrent anaplasmosis and/or babesiosis in pts w/ persistent fever; don’t use long-term abx for Post-tx Lyme Dz Syndrome (PTLDS) - If persistent fever >1 day on abx, assess for co-infxn w/ A phagocytophilum or B microti in pts who live where these organisms are endemic1
- If pt hx suggests reinfxn, offer repeat abx according to specific Lyme indications (eg, EM, carditis, etc); consider 2nd course of abx w/ alternate drug, if concern for tx failure2
- If Lyme arthritis improving but not resolved, use 2nd course of PO abx;3 if no/minimal response to initial PO abx, consider 2- to 4-wk course of IV ceftriaxone over 2nd course of PO abx;3,4 if pt fails PO and IV abx, consider DMARDs, biologic agents, interarticular steroids, or synovectomy5
CDC 2022 & IDSA/AAN/ACR: Recommended parenteral abx dosing/duration for PO abx refractory Lyme arthritis:1,3 PTLDS: Don’t give additional abx to pts w/ persistent fatigue, pain, or cognitive impairment but no objective s/sx of reinfxn or tx failure (eg, inflammatory arthritis, meningitis, neuropathy);5 most will improve w/ time (months – yrs);2,3 outcomes for these pts no better than placebo & long-term abx have been assoc w/ serious or fatal complications3,* Footnotes 1 IDSA/AAN/ACR 2020. Characteristic lab abnormalities in both anaplasmosis and babesiosis incl:
• thrombocytopenia
• leukopenia
• neutropenia
• anemia
Evidence of hemolysis (anemia, ↑indirect bili, ↑LDH) particularly suggestive of babesiosis.
Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
2 NICE 2018. Lyme Disease - NICE Guideline (NG95). National Institute for Health and Care Excellence. Published 4/11/18. Last updated 10/17/18. Accessed 5/31/23
3 CDC 2022. Lyme Disease. Last reviewed 1/19/22. Accessed 6/20/23
4 IDSA/AAN/ACR 2020. IDSA makes no recommendation (2nd-course abx vs observation) re: partial response to initial tx in Lyme arthritis. A 2nd course of PO abx may be a reasonable alt to IV abx in pts w/ modest synovial proliferation & those preferring PO over IV tx.
Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
5 IDSA/AAN/ACR 2020.
Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
* ILADS 2014. ILADS diverges from CDC, IDSA, & NICE in recognizing a persistent infxn state they define as “chronic Lyme disease,” and recommend that abx retreatment is “appropriate for the majority of pts who remain ill.” They recommend initial 4- to 6-wk course of abx (incl IV abx) be continued until pt has reached full recovery.
Cameron DJ, et al. Evidence Assessments and Guideline Recommendations in Lyme Disease: The Clinical Management of Known Tick Bites, Erythema migrans Rashes and Persistent Disease. Expert Rev Anti Infect Ther. 2014. Sept;12(9):1103-1135. Free full-text PDF @ PubMed® Central
Numerous groups, incl the Infectious Diseases Society of America (IDSA), have raised concern about the quality, validity, and inherent bias of International Lyme and Associated Diseases Society (ILADS) guidance, which does not meet epocrates editorial standards. We include their recommendations here not as an endorsement of their validity but to provide context when confronted w/ pt questions arising from ILADS recommendations. -
Asymptomatic pt, bitten by tick Prompt tick removal is important to ↓ Lyme risk. Don’t test tick, nor asymptomatic pt, for B burgdorferi. Don’t diagnose Lyme dz in asymptomatic pts.1 Abx ppx indicated in certain pts, while watch & wait is appropriate for others - Remove attached ticks ASAP by mechanical means using clean, fine-tipped tweezer (or a comparable device) inserted btwn tick body and skin;2 transmission occurs after 36-48h of attachment3,4
- Don’t use heat/match, nail polish, petrolatum, or other chemicals to force tick to detach; this may delay removal3 or cause tick to regurgitate and potentially ↑ risk of pathogen transmission4
- Send tick to lab for species ID, per IDSA;4 CDC makes no recommendation re: lab ID3,5
- Don’t test tick for B burgdorferi;3,4 (+) result poorly predicts clinical infxn or asymptomatic seroconversion3
- Provide abx ppx w/in 72h of removal, only to pts w/ an identified high-risk tick bite:6,7 doxycycline 200 mg PO x1 for adults or 4.4 mg/kg/dose (max 200 mg) for children;4,5,* watch & wait appropriate for pts w/ low or equivocal risk4,5
- Monitor for erythema migrans (EM) or other s/sx of tick-borne infxn in wks following tick bite; avg onset of EM: 7 days after bite (range: 3-90 days);1,3 STARI rash looks similar but occurs slightly earlier, after Amblyomma americanum bite;8 an earlier inflammatory reaction may wax & wane at bite site w/in first 48h, not representative of EM or Lyme1,5
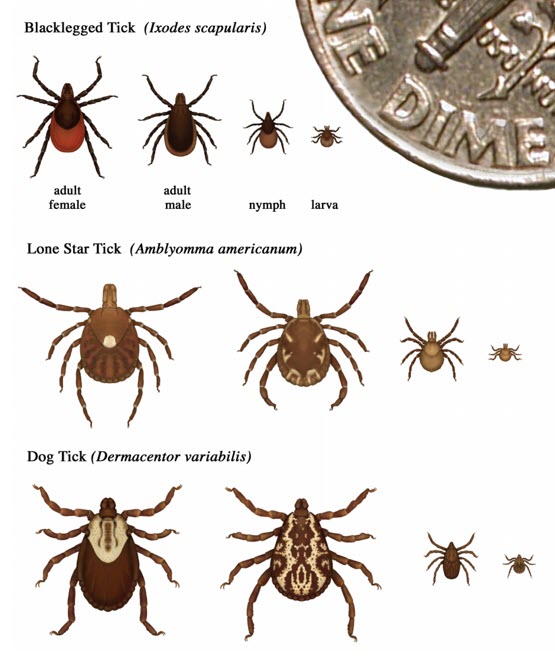
Ticks that commonly bite humans:5 Footnotes 1 NICE 2018. Lyme Disease - NICE Guideline (NG95). National Institute for Health and Care Excellence. Published 4/11/18. Last updated 10/17/18. Accessed 5/31/23
2 CDC 2022. Tick removal technique:
• Use clean, fine-tipped tweezers to grasp the tick as close to the skin’s surface as possible.
• Pull upward w/ steady, even pressure. Don’t twist or jerk the tick; if mouth-parts break off and remain in the skin, remove the mouth-parts w/ tweezers. If unable to remove the mouth easily w/ tweezers, leave it alone and let the skin heal.
• After removing the tick, thoroughly clean the bite area and your hands w/ rubbing alcohol or soap and water.
• Dispose of a live tick by putting it in alcohol, placing it in a sealed bag/container, wrapping it tightly in tape, or flushing it down the toilet.
Lyme Disease: Tick removal and testing. Last reviewed 5/13/22. Accessed 6/21/23
3 CDC 2022. Lyme Disease. Last reviewed 1/19/22. Accessed 6/20/23
4 IDSA/AAN/ACR 2020. Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
5 CDC 2021. Ticks. Last reviewed 10/21/21. Accessed 6/21/23
6 IDSA/AAN/ACR 2020. High-risk tick bite (all must be true): the tick bite was from (a) an identified Ixodes spp. vector species, (b) it occurred in a highly endemic area, and (c) the tick was attached for ≥36h.
Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
7 CDC 2021. High-risk tick bite (all must be true):
(a) the tick bite occurred in a state where Lyme dz incidence is high, or in an area where >20% of ticks are infected w/ Borrelia burgdorferi;
(b) the attached tick can be identified as an adult or nymphal blacklegged tick;
(c) the estimated time of attachment is ≥36h based on degree of tick engorgement w/ blood ( CDC image) or likely time of exposure to the tick.
Guidance for Clinicians: Caring for Patients after a Tick Bite. December 14, 2021. Accessed 6/21/23
8 CDC 2018. Southern Tick–Associated Rash Illness: STARI or Lyme? Last reviewed 11/19/18. Accessed 6/21/23
* ILADS 2014. ILADS diverges from CDC & IDSA guidance, recommending against single-dose doxycycline, instead recommending: “Clinicians should promptly offer abx ppx for all Ixodes tick bites in which there is evidence of tick feeding, regardless of the degree of tick engorgement or the infection rate in the local tick population. The preferred regimen is doxycycline 100–200 mg bid x20 days. Other treatment options may be appropriate on an individualized basis.” They cite very low-quality evidence, and differing values leading to a differing conclusion upon evaluation of that evidence.
Cameron DJ, et al. Evidence Assessments and Guideline Recommendations in Lyme Disease: The Clinical Management of Known Tick Bites, Erythema migrans Rashes and Persistent Disease. Expert Rev Anti Infect Ther. 2014. Sept;12(9):1103-1135. Free full-text PDF @ PubMed® Central
Numerous groups, incl the Infectious Diseases Society of America (IDSA), have raised concern about the quality, validity, and inherent bias of International Lyme and Associated Diseases Society (ILADS) guidance, which does not meet epocrates editorial standards. We include their recommendations here not as an endorsement of their validity but to provide context when confronted w/ pt questions arising from ILADS recommendations.
Pt w/ other conditions or sx atypical for Lyme dz In endemic area, consider Lyme dz in pts w/ certain sx or conditions, even in absence of distinct tick bite - Use combo of clinical presentation (sx, h/o possible tick exposure) and lab testing to guide dx & tx of pts w/o erythema migrans (EM);1,2 consider starting tx while awaiting labs2
- Consider Lyme (or other tick-borne illness)3 in absence of EM in pts w/ acute onset of multiple sx: fever, sweats, lymphadenopathy, malaise, fatigue, neck pain/stiffness, migratory joint or muscle pain, cognitive impairment, HA, paresthesia;* inquire about possible tick exposure; also consider Lyme in pts w/ eye sx (eg, uveitis, keratitis)2
- Perform 2-tier testing when Lyme being considered in absence of EM: initial ELISA1,2 or IFA,1 then Western immunoblot (or FDA-approved 2nd EIA4) if 1st test is (+) or equivocal; don’t r/o dx if tests are (-) but there’s high clinical suspicion of Lyme dz2
- In pts w/ potential tick exposure in a Lyme dz–endemic area who have 1+ skin lesions suggestive of, but atypical for, EM, consider Ab testing performed on an acute-phase serum sample, followed by a convalescent-phase serum sample (2-3wk later) if initial result is (-)5
- Don’t use unaccredited labs or unvalidated tests for Lyme dx2,6,**
Consider testing for Lyme dz in limited pts being evaluated for other conditions - If appropriate epidemiologic setting, test for Lyme in pts w/ unexplained carditis; in pts w/ chronic cardiomyopathy, IDSA suggests against routine testing for Lyme5
- Don’t test pts w/ amyotrophic lateral sclerosis, relapsing-remitting multiple sclerosis, Parkinson dz, dementia or cognitive decline, new-onset seizures, or other atypical neuro conditions for Lyme5,***
- Don’t test adults w/ psych illness for Lyme, per IDSA (NICE says to consider doing so);* consider not testing kids w/ developmental, behavioral, or psych disorders5
- In pts w/ nonspecific white matter changes on brain imaging w/o hx of other clinical or epidemiologic support for the dx of Lyme dz, IDSA suggests against testing for Lyme, while NICE suggests testing can be considered
Footnotes 1 CDC 2022. Lyme Disease. Last reviewed 1/19/22. Accessed 6/20/23
2 NICE 2018. Lyme Disease - NICE Guideline (NG95). National Institute for Health and Care Excellence. Published 4/11/18. Last updated 10/17/18. Accessed 5/31/23
3 CDC 2021. Ticks: Symptoms of Tickborne Illness. Last reviewed 8/5/21. Accessed 6/22/23
4 CDC 2019. Mead P, et al. Updated CDC Recommendation for Serologic Diagnosis of Lyme Disease. Morb Mortal Wkly Rep. 2019;68:703. PDF
5 IDSA/AAN/ACR 2020. Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
6 CDC 2023. Examples of unvalidated tests include:
• Capture assays for antigens in urine
• Immunofluorescence staining, or cell sorting of cell wall–deficient or cystic forms of B burgdorferi
• Lymphocyte transformation tests
• Quantitative CD57 lymphocyte assays
• “Reverse Western blots”
• In-house criteria for interpretation of FDA-cleared tests
• IgM or IgG tests w/o previous enzyme immunoassay
Lyme Disease: Laboratory tests and practices that are not currently recommended. Last reviewed 2/9/23. Accessed 6/20/23
* ILADS 2021. ILADS diverges from IDSA and CDC, recognizing “chronic Lyme disease” as an active infxn lasting years (or decades) and causing common sx such as: fatigue, cognitive dysfxn, HA, sleep disturbances, migratory arthralgia & myalgia, numbness & tingling, neuropathic pain, anxiety & depression, and musculoskeletal problems.
Lyme Disease Basics for Providers: A Brief Primer by International Lyme and Associated Diseases Society. Accessed 5/31/21
Numerous groups, incl the Infectious Diseases Society of America (IDSA), have raised concern about the quality, validity, and inherent bias of International Lyme and Associated Diseases Society (ILADS) guidance, which does not meet epocrates editorial standards. We include their recommendations here not as an endorsement of their validity but to provide context when confronted w/ pt questions arising from ILADS recommendations.
** ILADS 2021. ILADS diverges from CDC and NICE guidance, supporting “emerging testing modalities” that “present new opportunities for addressing the challenges faced in lab eval of Lyme dz.”
Numerous groups, incl the Infectious Diseases Society of America (IDSA), have raised concern about the quality, validity, and inherent bias of International Lyme and Associated Diseases Society (ILADS) guidance, which does not meet epocrates editorial standards. We include their recommendations here not as an endorsement of their validity but to provide context when confronted w/ pt questions arising from ILADS recommendations.
*** ILADS 2021. ILADS diverges from IDSA guidance, claiming that Lyme should be considered in the diff dx of rheumatologic and neurologic conditions, as well as chronic fatigue syndrome, fibromyalgia, somatization disorder, and “any difficult-to-diagnose multi-system illness.”
Numerous groups, incl the Infectious Diseases Society of America (IDSA), have raised concern about the quality, validity, and inherent bias of International Lyme and Associated Diseases Society (ILADS) guidance, which does not meet epocrates editorial standards. We include their recommendations here not as an endorsement of their validity but to provide context when confronted w/ pt questions arising from ILADS recommendations.
No sx or concerns, pt wants to prevent Lyme dz Use personal protective measures, repellants, & tick checks to ↓ risk of tick exposure & infxn w/ tick-borne illness - Wear light-colored, long-sleeved/legged clothing to make ticks more apparent before attachment1,2
- Tuck pants into socks to prevent ticks from attaching to skin of ankles & legs; keep to center of trail, avoid wooded & brushy areas w/ high grass and leaf litter1-3
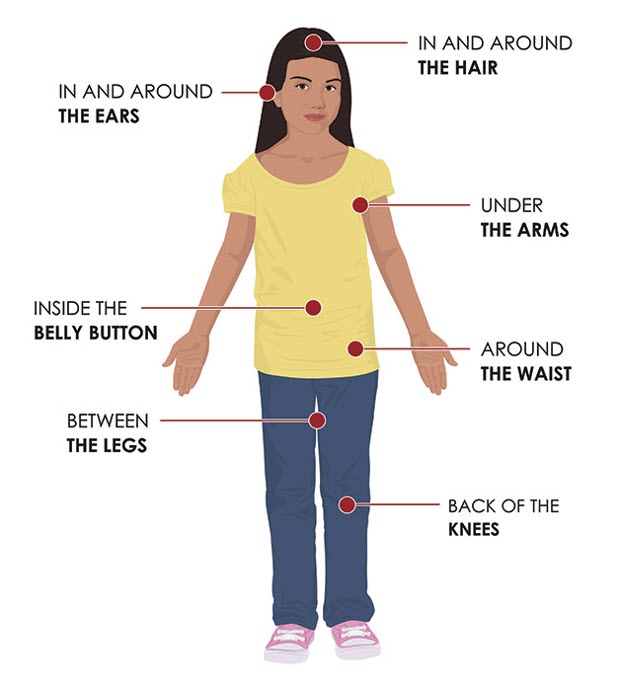
- Perform full-body tick check after being outdoors;3 bathing/showering w/in 2h of outdoor activity significantly ↓ risk of Lyme dz2,3
- Put clothes in hot dryer for 10min, or wash clothes in hot (not warm or cold) water, to kill ticks2,3
- Check gear,1 companion animals, for unattached ticks1,2
- Repellants recommended for skin & clothing: N,N-Diethyl-meta-toluamide (DEET),4 picaridin, ethyl-3-(N-n-butyl-N-acetyl) aminopropionate (IR3535), oil of lemon eucalyptus (OLE),5 p-methane-3,8-diol (PMD),5 2-undecanone3
- Permethrin spayed on or impregnated in clothing kills ticks on contact, is more effective than DEET2,3
- Not recommended: botanical agents & essential oils (eg, essential oils of rosemary, cinnamon leaf, lemongrass, geraniol, nootkatone, and carvacrol)2
Full-body tick check points3 Footnotes 1 CDC 2017. Travelers’ Health: Diseases Spread by Ticks. Last reviewed 10/23/17. Accessed 6/22/23
2 IDSA/AAN/ACR 2020. Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
3 CDC 2019. Lyme Disease: Preventing Tick Bites on People. Last reviewed 9/30/19. Accessed 6/22/23
4 IDSA/AAN/ACR 2020. The EPA has approved DEET for use on children, w/ no age restriction. Because of a lack of safety data, however, the AAP & CDC only recommend DEET for children >2 mo of age.
Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
5 IDSA/AAN/ACR 2020. The AAP, CDC, and EPA do not recommend OLE and PMD for children <3 yo.
Lantos PM, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021. Jan 23;72(1):1-8. Accessed 5/31/23
|