-
Severity classification/Initiating tx
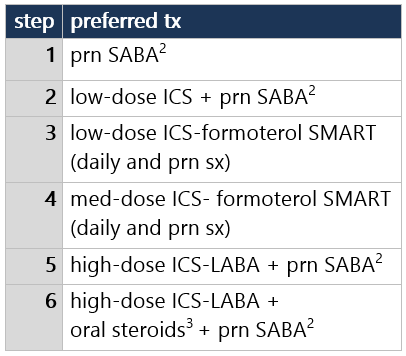
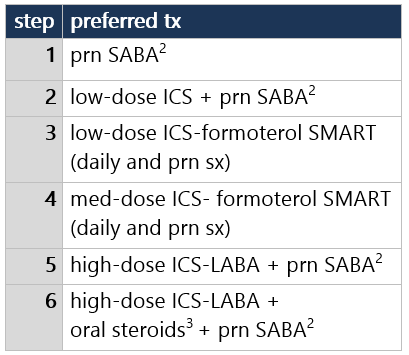
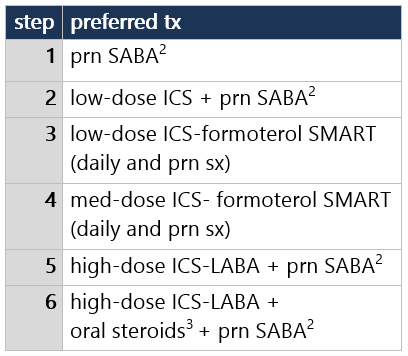
All of: Sx/SABA use not every day, not more than once/day, sx ≤4 nights/mo, no/minor activity limits, FEV1 >80%, FEV1/FVC >80% Intermittent | All of: Sx/SABA use ≤2 days/wk, sx ≤2 nights/mo, no activity limits, FEV1/FVC >85%, ≤1 exac/yr requiring PO/IV steroids Step 1 for Intermittent dz1,2 = SABA prn - SABA (albuterol, levalbuterol)3 prn
- SABA use for sx >2 days/wk indicates inadequate control (except EIB use)4
Offer action plan + pt ed, F/U in 2-6wk - Written action plan based on sx or peak flow
- Educate: sx, meds, inhaler technique, environment control,5 comorbidity6 mgmt
- F/U q2–6wk while gaining control, then q1–6mo to monitor control
- Spirometry1 q1-2yrs (more frequently if not well controlled)
- Inactivated flu vaccine annually
Footnotes 1 Intermittent dz = sx/SABA use ≤2 days/wk, sx ≤2 nights/mo, no interference w/ NL activity, NL FEV1 between exac, FEV1 >80%, FEV1/FVC >85%; ≤1 exac/yr requiring PO/IV steroids (inadequate data to correlate exac freq w/ severity). Dx: hx/exam to determine sx d/t recurrent airway obstruction: cough, recurrent wheeze/difficult breathing/chest tightness worse @ night or w/ exercise, viral infxn, allergens/irritants, weather, laugh/cry, stress, etc. ✓ spirometry to determine at least partial reversibility.
2 Differential Dx: Allergic rhinitis, sinusitis, foreign body, vocal cord dysfxn, bronchostenosis, LN/tumor, viral or obliterative bronchiolitis, CF, heart dz, aspiration.
3 Available SABAs (in alpha order):
• albuterol MDI 90 mcg 2 puffs q4-6h prn
• albuterol NEB 1.25-5 mg in 3 cc saline q4-8h prn
• levalbuterol MDI 45 mcg 2 puffs q4-6h prn
• levalbuterol NEB 0.31-0.63 mg q8h prn
If SABA not tolerated, ipratropium may be used as alternative.
4 SABA >2x/wk indicates poor control except for EIB pre-exercise prevention. Encourage full participation in physical activities. If cold-induced EIB: Warm-up period or mask/scarf over mouth.
5 Allergens, irritants, pollutants: ✓ hx exposure-related sx. Avoid tobacco smoke.
6 Identify comorbidities: rhinitis, sinusitis, GERD, obesity, OSA, ABPA, stress, depression, etc.
Mild persistent | Any of: Sx/SABA use >2 days/wk or sx 3-4 nights/mo or minor activity limits or FEV1/FVC ≤85% or 2+ exac/yr requiring PO/IV steroids Step 2 for Mild Persistent dz1,2 = Daily controller meds + prn SABA - Daily low-dose ICS preferred. Alternatives: LTRA, cromolyn, nedocromil, or theophylline
- Plus SABA (albuterol, levalbuterol)3 prn
- SABA use for sx >2 days/wk indicates inadequate control (except EIB use)4
- Determine allergen exposure; consider immuno-tx SC for persistent allergic asthma5
Offer action plan + pt ed, F/U in 2-6wk - Written action plan based on sx or peak flow
- Educate: sx, meds, inhaler technique, environment control,6 comorbidity7 mgmt
- F/U q2–6wk while gaining control, q1–6mo to monitor control, q3mo if step-down tx anticipated
- Spirometry1 q1-2yrs (more frequently if not well controlled)
- May use FeNO as part of monitoring (w/ hx, clinical findings, spirometry) in pts w/ persistent allergic asthma
- Inactivated flu vaccine annually
Footnotes 1 Mild Persistent = sx/SABA use >2 days/wk not daily or more than once/day, sx 3-4 nights/mo, minor limitations to NL activity, FEV1 >80%, FEV1/FVC >80%, ≥2 exac/yr requiring PO/IV steroids (inadequate data to correlate exac freq w/ severity; but ≥2/yr considered persistent despite impairment level). Dx: hx/exam to determine sx d/t recurrent airway obstruction: cough, recurrent wheeze/difficult breathing/chest tightness worse @ night or w/ exercise, viral infxn, allergens/irritants, weather, laugh/cry, stress, etc ✓ spirometry to determine at least partially reversibility.
2 Differential Dx: Allergic rhinitis, sinusitis, foreign body, vocal cord dysfxn, bronchostenosis, LN/tumor, viral or obliterative bronchiolitis, CF, heart dz, aspiration.
3 Available SABAs (in alpha order):
• albuterol MDI 90 mcg 2 puffs q4-6h prn
• albuterol NEB 1.25-5 mg in 3 cc saline q4-8h prn
• levalbuterol MDI 45 mcg 2 puffs q4-6h prn
• levalbuterol NEB 0.31-0.63 mg q8h prn
If SABA not tolerated, ipratropium may be used as alternative. Theophylline less desirable d/t level monitoring.
4 SABA >2x/wk indicates poor control except for EIB pre-exercise prevention. Encourage full participation in physical activities. If cold-induced EIB: Warm-up period or mask/scarf over mouth.
5 Allergens, irritants, pollutants: ✓ hx exposure-related sx. Avoid tobacco smoke. If persistent asthma, use skin/in vitro tests for perennial indoor allergens. If clear connection b/t sx and allergen, consider immuno-tx by trained personnel; immuno-tx requires preparation to tx anaphylaxis. Evidence best for dust mite, animal dander, pollen; evidence weak/lacking for molds, cockroaches; evidence strongest for single-allergen immuno-tx.
6 Identify comorbidities: rhinitis, sinusitis, GERD, obesity, OSA, ABPA, stress, depression, etc.
Any of: Sx/SABA use every day or more than once/day or sx >1 night/wk or some activity limits or FEV1 ≤80% or FEV1/FVC ≤80% Moderate persistent | All of: Sx/SABA use not throughout day, sx not every night, no extreme activity limits, FEV1 ≥60%, FEV1/FVC ≥75% Step 3 for Moderate Persistent dz1,2 = Daily and prn low-dose ICS-formoterol - Use single-inhaler maintenance & reliever tx (SMART): low-dose ICS-formoterol daily & prn sx (max 8 puffs/day=36 mcg formoterol)
- Alternatives (w/ prn SABA):3 med-dose ICS; low-dose ICS-LABA; low-dose ICS + LTRA; low-dose ICS + theophylline
- SABA use for sx >2 days/wk indicates inadequate control (except EIB use)4
- Consider short-course PO steroids5
- Determine allergen exposure; consider immuno-tx SC for persistent allergic asthma6
Offer action plan + pt ed, F/U in 2-6wk - Written action plan based on sx or peak flow; consider daily peak flow monitoring
- Educate: sx, meds, inhaler technique, environment control,6 comorbidity7 mgmt
- F/U q2–6wk while gaining control, q1–6mo to monitor control, q3mo if step-down tx anticipated; consider asthma specialist consult
- Spirometry1 q1-2yrs (more frequently if not well controlled)
- May use FeNO as part of monitoring (w/ hx, clinical findings, spirometry) in pts w/ persistent allergic asthma
- Inactivated flu vaccine annually
Footnotes 1 Mod Persistent = daily sx/SABA use (but not throughout day), night sx >1x/wk but not nightly, some limitations to NL activity but not extreme, FEV1 60%-80%, FEV1/FVC 75%-80%, ≥2 exac/yr requiring PO/IV steroids (inadequate data to correlate exac freq w/ severity; but ≥2/yr considered persistent despite impairment level). Dx: hx/exam to determine sx d/t recurrent airway obstruction: cough, recurrent wheeze/difficult breathing/chest tightness worse @ night or w/ exercise, viral infxn, allergens/irritants, weather, laugh/cry, stress, etc. ✓ spirometry to determine at least partial reversibility.
2 Differential Dx: Allergic rhinitis, sinusitis, foreign body, vocal cord dysfxn, bronchostenosis, LN/tumor, viral or obliterative bronchiolitis, CF, heart dz, aspiration.
3 Available SABAs (in alpha order):
• albuterol MDI 90 mcg 2 puffs q4-6h prn
• albuterol NEB 1.25-5 mg in 3 cc saline q4-8h prn
• levalbuterol MDI 45 mcg 2 puffs q4-6h prn
• levalbuterol NEB 0.31-0.63 mg q8h prn
If SABA not tolerated, ipratropium may be used as alternative. Theophylline less desirable d/t level monitoring.
4 SABA >2x/wk indicates poor control except for EIB pre-exercise prevention. LTRAs, cromolyn, or LABAs also protect in EIB. Frequent/chronic LABA to prevent EIB discouraged (may disguise poorly controlled persistent dz). Consider long-term controllers; EIB often marks inadequate control and responds to regular anti-inflammatory tx. Encourage full participation in physical activities. If cold-induced EIB: Warm-up period or mask/scarf over mouth.
5 Oral steroids (options listed in EPR-3 Quick Reference 2012, in alpha order): methylprednisolone, prednisolone, or prednisone: 0.25-2 mg/kg daily (single AM dose) or every other day as needed for control. Short-course burst to gain control: 1-2 mg/kg/day (max 60 mg/day) x3–10 days.
6 Allergens, irritants, pollutants: ✓ hx exposure-related sx. Avoid tobacco smoke. If persistent asthma, use skin/in vitro tests for perennial indoor allergens. If clear connection b/t sx and allergen, consider immuno-tx by trained personnel. Evidence best for dust mite, animal dander, pollen; evidence weak/lacking for molds, cockroaches; evidence strongest for single-allergen immuno-tx.
7 Identify comorbidities: rhinitis, sinusitis, GERD, obesity, OSA, ABPA, stress, depression, etc.
Severe persistent | Any of: Sx/SABA use throughout day or sx 7 nights/wk or extreme activity limits or FEV1 <60% or FEV1/FVC <75% Step 3/4 for Severe Persistent dz1,2 = Med-dose ICS alone or in combo w/ formoterol - Use single-inhaler maintenance & reliever tx (SMART) as Step 4 preference: med-dose ICS-formoterol daily & prn sx (max 8 puffs/day=36 mcg formoterol)
- Alternatives (w/ prn SABA):3 med-dose ICS (Step 3); med-dose ICS-LABA (Step 4); med-dose ICS + LTRA (Step 4); med-dose ICS + theophylline (Step 4)
- SABA use for sx >2 days/wk indicates inadequate control (except EIB use)4
- Consider short-course PO steroids5
- Determine allergen exposure; consider immuno-tx SC for persistent allergic asthma6
Offer action plan + pt ed, F/U in 2-6wk - Written action plan based on sx or peak flow; consider daily peak flow monitoring
- Educate: sx, meds, inhaler technique, environment control,6 comorbidity7 mgmt
- F/U q2–6wk while gaining control, q1–6mo to monitor control, q3mo if step-down tx anticipated
- Asthma specialist consult required at Step 4 (consider at Step 3)
- Spirometry1 q1-2yrs (more frequently if not well controlled)
- May use FeNO as part of monitoring (w/ hx, clinical findings, spirometry) in pts w/ persistent allergic asthma
- Inactivated flu vaccine annually
Footnotes 1 Severe Persistent = sx/SABA use throughout day, night sx often 7x/wk, extreme limitations to NL activity, FEV1 <60%, FEV1/FVC <75%, ≥2 exac/yr requiring PO/IV steroids (inadequate data to correlate exac freq w/ severity; but ≥2/yr considered persistent despite impairment level). Dx: hx/exam to determine sx d/t recurrent airway obstruction: cough, recurrent wheeze/difficult breathing/chest tightness worse @ night or w/ exercise, viral infxn, allergens/irritants, weather, laugh/cry, stress, etc. ✓ spirometry to determine at least partial reversibility.
2 Differential Dx: Allergic rhinitis, sinusitis, foreign body, vocal cord dysfxn, bronchostenosis, LN/tumor, viral or obliterative bronchiolitis, CF, heart dz, aspiration.
3 Available SABAs (in alpha order):
• albuterol MDI 90 mcg 2 puffs q4-6h prn
• albuterol NEB 1.25-5 mg in 3 cc saline q4-8h prn
• levalbuterol MDI 45 mcg 2 puffs q4-6h prn
• levalbuterol NEB 0.31-0.63 mg q8h prn
If SABA not tolerated, ipratropium may be used as alternative. Theophylline less desirable d/t level monitoring.
4 SABA >2x/wk indicates poor control except for EIB pre-exercise prevention. LTRAs, cromolyn, or LABAs also protect in EIB. Frequent/chronic LABA to prevent EIB discouraged (may disguise poorly controlled persistent dz). Consider long-term controllers; EIB often marks inadequate control and responds to regular anti-inflammatory tx. Encourage full participation in physical activities. If cold-induced EIB: Warm-up period or mask/scarf over mouth.
5 Oral steroids (options listed in EPR-3 Quick Reference 2012, in alpha order): methylprednisolone, prednisolone, or prednisone: 0.25-2 mg/kg daily (single AM dose) or every other day as needed for control. Short-course burst to gain control: 1-2 mg/kg/day (max 60 mg/day) x3–10 days.
6 Allergens, irritants, pollutants: ✓ hx exposure-related sx. Avoid tobacco smoke. If persistent asthma, use skin/in vitro tests for perennial indoor allergens. If clear connection b/t sx and allergen, consider immuno-tx by trained personnel. Evidence best for dust mite, animal dander, pollen; evidence weak/lacking for molds, cockroaches; evidence strongest for single-allergen immuno-tx.
7 Identify comorbidities: rhinitis, sinusitis, GERD, obesity, OSA, ABPA, stress, depression, etc.
-
Follow-up: Control assessment/tx adjustment
Well-controlled | All of: Sx/SABA use ≤2 days/wk, ≤1x/day, sx ≤1 night/mo, no activity limits, ≤1 exac/yr requiring PO/IV steroids, w/ FEV1 >80%, FEV1/FVC >80% Maintain current tx step for well-controlled dz;1 consider step down if well controlled1 for ≥3 mo Educate + F/U - F/U q1–6mo to monitor control, q3mo if step-down tx anticipated
- Spirometry q1–2yrs
- Inactivated flu vaccine annually
- Every visit: Reinforce self-monitoring (sx or peak flow), action plan, inhaler/device technique, quick-relief vs controller meds, med adherence, environment control
- Encourage/praise to build confidence
Footnotes 1 Well controlled = sx/SABA use ≤2 days/wk, sx ≤2 nights/mo, no interference w/ NL activity, FEV1 >80%, ≤1 exac/yr requiring PO/IV steroids (inadequate data to correlate exac freq w/ control). Most important determinant of dosing = clinician judgment of response to tx: sx, activity level, lung fxn.
2 Available SABAs (in alpha order):
• albuterol MDI 90 mcg 2 puffs q4-6h prn
• albuterol NEB 1.25-5 mg in 3 cc saline q4-8h prn
• levalbuterol MDI 45 mcg 2 puffs q4-6h prn
• levalbuterol NEB 0.31-0.63 mg q8h prn
3 Oral steroids (options listed in EPR-3 Quick Reference 2012, in alpha order): methylprednisolone, prednisolone, or prednisone: 0.25-2 mg/kg daily (single AM dose) or every other day as needed for control. Short-course burst to gain control: 1-2 mg/kg/day (max 60 mg/day) x3–10 days. Inadequately controlled | Any of: Sx/SABA use >2 days/wk or >1x/day or sx ≥2 nights/mo or activity limits or 2+ exac/yr requiring PO/IV steroids or FEV1 ≤80% or FEV1/FVC ≤80% Not well controlled | All of: Sx/SABA use not throughout day, sx <2 nights/wk, no extreme activity limits, FEV1 ≥60%, FEV1/FVC ≥75% Step up at least 1 tx step for not-well-controlled dz;1 1st review adherence, inhaler technique, environment control - If alternative tx used, switch to preferred tx for current step. If side effects, consider alternative tx
- If persistent, allergic asthma: consider SC immuno-tx (strongest evidence for single-allergen tx; evidence weak/lacking for mold/cockroach)
- If Step 5 or 6, consider omalizumab
Educate + F/U in 2wk to achieve control - F/U q2–6wk to achieve control, then q1–6mo to monitor control, q3mo if step-down tx anticipated
- Consult asthma specialist for Steps ≥4; consider at Step 3
- Spirometry q1–2yrs (more frequently if not well controlled)
- May use FeNO as part of monitoring (w/ hx, clinical findings, spirometry) in pts w/ persistent allergic asthma
- Inactivated flu vaccine annually
- Every visit: Reinforce self-monitoring (sx or peak flow), action plan, inhaler/device technique, quick-relief vs controller meds, med adherence, environment control
- Encourage/praise to build confidence
Footnotes 1 Not well controlled = sx/SABA use >2 days/wk (but not throughout day), sx 1-3 nights/wk, some limitations to NL activity, FEV1 60%-80%, ≥2 exac/yr requiring PO/IV steroids (inadequate data to correlate exac freq w/ control; but more frequent/more intense exacs indicate poorer asthma control). Most important determinant of dosing = clinician judgment of response to tx: sx, activity level, lung fxn.
2 Available SABAs (in alpha order):
• albuterol MDI 90 mcg 2 puffs q4-6h prn
• albuterol NEB 1.25-5 mg in 3 cc saline q4-8h prn
• levalbuterol MDI 45 mcg 2 puffs q4-6h prn
• levalbuterol NEB 0.31-0.63 mg q8h prn
3 Oral steroids (options listed in EPR-3 Quick Reference 2012, in alpha order): methylprednisolone, prednisolone, or prednisone: 0.25-2 mg/kg daily (single AM dose) or every other day as needed for control. Short-course burst to gain control: 1-2 mg/kg/day (max 60 mg/day) x3–10 days. Very poorly controlled | Any of: Sx/SABA use throughout day or sx ≥2 nights/wk or extreme activity limits or FEV1 <60% or FEV1/FVC <75% Consider short-course PO steroids. Step up 1-2 tx step(s) for very poorly controlled dz;1 1st review adherence, inhaler technique, environment control - If alternative tx used, switch to preferred tx for current step. If side effects, consider alternative tx
- If persistent, allergic asthma: consider SC immuno-tx (strongest evidence for single-allergen tx; evidence weak/lacking for mold/cockroach)
- If Step 5 or 6, consider omalizumab
Educate + F/U in 2wk to achieve control - F/U q2–6wk to achieve control, then q1–6mo to monitor control, q3mo if step-down tx anticipated
- Consult asthma specialist for Steps ≥4; consider at Step 3
- Spirometry q1–2yrs (more frequently if not well controlled)
- May use FeNO as part of monitoring (w/ hx, clinical findings, spirometry) in pts w/ persistent allergic asthma
- Inactivated flu vaccine annually
- Every visit: Reinforce self-monitoring (sx or peak flow), action plan, inhaler/device technique, quick-relief vs controller meds, med adherence, environment control
- Encourage/praise to build confidence
Footnotes 1 Very poorly controlled = sx/SABA use throughout day, sx ≥2 nights/wk, extreme limitations to NL activity, FEV1 <60%, ≥2 exac/yr requiring PO/IV steroids (inadequate data to correlate exac freq w/ control; but more frequent/more intense exacs indicate poorer asthma control). Most important determinant of dosing = clinician judgment of response to tx: sx, activity level, lung fxn.
2 Available SABAs (in alpha order):
• albuterol MDI 90 mcg 2 puffs q4-6h prn
• albuterol NEB 1.25-5 mg in 3 cc saline q4-8h prn
• levalbuterol MDI 45 mcg 2 puffs q4-6h prn
• levalbuterol NEB 0.31-0.63 mg q8h prn
3 Oral steroids (options listed in EPR-3 Quick Reference 2012, in alpha order): methylprednisolone, prednisolone, or prednisone: 0.25-2 mg/kg daily (single AM dose) or every other day as needed for control. Short-course burst to gain control: 1-2 mg/kg/day (max 60 mg/day) x3–10 days.
|